A Twenty-five-Year-Old Man with Right Knee Pain
January 19, 2011
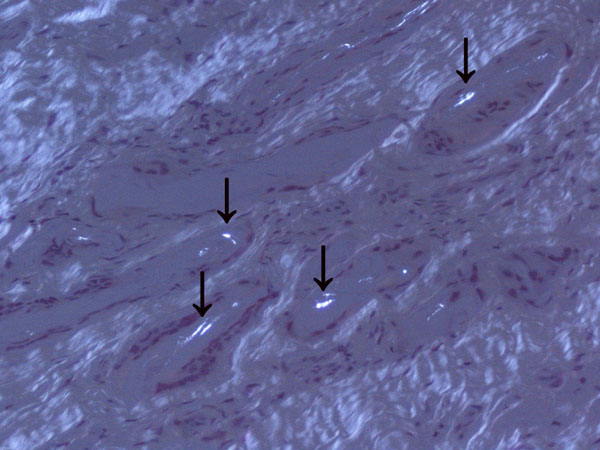
A twenty-five-year-old competitive soccer player initially presented at another hospital with a two-year history of right knee pain. He had persistent symptoms despite treatment with physical therapy, anti-inflammatory drugs, and rest. A computed tomography scan of the right knee was reported to show an osteochondral defect of the medial femoral condyle. The patient underwent arthroscopic autologous osteochondral transplantation to treat a full-thickness osteochondral defect of the medial femoral condyle of the right knee. The right knee pain was not relieved, however, and he did not return to sports activity. When the patient was seen at our institution four years after this initial surgery, he walked with a limp. Physical examination revealed signs of patellofemoral joint abnormality. The results of the step up-step down test, patellofemoral grinding test, and patellofemoral compression test were all positive. The range of motion of the knee included an extension lag of 5° but full knee flexion. All biochemical and serologic tests were normal, with no signs of inflammation or increased bone metabolism. Radiographs showed a radiolucent area in the medial aspect of the right trochlea (Fig. 1). Magnetic resonance imaging showed an osteochondral defect at the donor site, in the medial aspect of the femoral trochlea (Fig. 2). The patient underwent further arthroscopy of the knee. The area of the previous osteochondral implant, in the right medial femoral condyle, appeared healed on arthroscopic inspection, and a biopsy revealed hyaline cartilage in the implant zone. During the arthroscopy, a soft lesion in the medial aspect of the trochlea, corresponding to the previous donor site, was detected. The lesion was palpated with a probe, and it started to bleed (Fig. 3). A needle biopsy of the lesion was performed (Fig. 4).
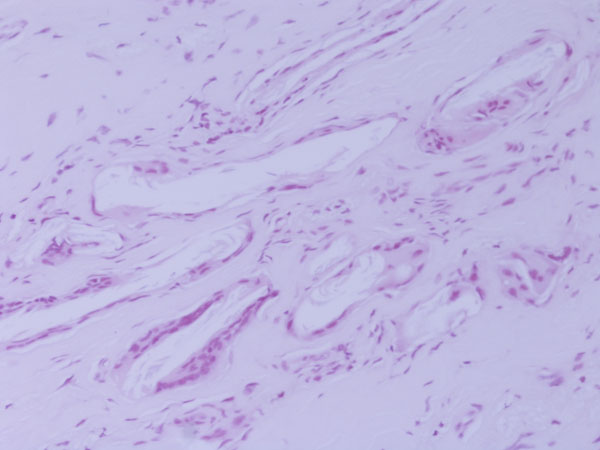
Histologically, the lesion was shown to be a foreign-body reaction. The histology slides were viewed with polarized light, which revealed small shards of birefringent material occupying the empty spaces in the tissue. Not enough material was present to define the condition more specifically (Fig. 5). The defect was curetted and, during the same revision arthroscopy, an osteochondral grafting procedure was performed with use of an osteochondral donor graft harvested from the lateral femoral condyle. A histological diagnosis was not made before placement of the plug. Postoperatively, the knee was immobilized for two weeks with a soft knee brace, and partial weight-bearing was allowed the day after the arthroscopy. Three weeks after surgery, range-of-motion exercises were started with use of a continuous passive-motion device. Full weight-bearing was permitted beginning four weeks after surgery. The symptoms resolved unremarkably. Physical examination revealed negative patellofemoral signs. A step up-step down test, patellofemoral grinding test, and patellofemoral compression test were negative. The patient returned to sports activity, but not at the previous competitive level. At the follow-up visit two years postoperatively, the patient was fully active, walked normally, and had a Lysholm score of 99.
Proceed to Discussion >>Reference: Longo UG, Franceschi F, Ruzzini L, Rabitti C, Maffulli N, Denaro V. Foreign-body giant-cell reaction at the donor site after autologous osteochondral transplant for cartilaginous lesion. A case report. J Bone Joint Surg Am. 2009;91:945-9.
Many open and arthroscopic techniques for chondrocyte transplantation have been described. No optimal standard technique exists for cartilage repair, and no well-conducted, adequately powered long-term studies are available to fully evaluate the various procedures. Osteochondral autograft transfer is an effective method for the management of patients with symptomatic full-thickness chondral defects of the femoral condyles, and it has several advantages. Firstly, because the hyaline cartilage is harvested in the form of osteochondral grafts during the index procedure, the technique does not depend on chondrocyte proliferation, matrix implantation, or mesenchymal cell differentiation for the restoration of articular cartilage. The method is not laboratory dependent, involves only a one-stage procedure, is of low cost, and carries no risk of disease transmission or immunologically mediated damage to the graft. Also, osteochondral autograft transfer is a minimally invasive procedure that can be performed through a small incision or even arthroscopically. Concerns remain in relation to the morbidity that ensues at the donor cartilage harvest sites. Morbidity of the donor sites can be an insidious pitfall of osteochondral autograft transfer. During osteochondral autograft transfer procedures, cylindrical transplants are harvested from the less weight-bearing areas of the femoral condyles, and the harvest sites are routinely left empty. Normally, natural healing processes originating in the cellular elements of the subchondral bone marrow result in fibrocartilage coverage of these harvest sites. These donor sites are filled by cancellous bone in four weeks and covered by initial repair tissue in six weeks, and fibrocartilage coverage develops within eight to twelve weeks. Typical donor sites are not free of disadvantages: grafts taken from the concave central intercondylar notch lack the ability to accurately restore the normal surface anatomy of convex regions. The generally lower pressure on the distal medial portion of the trochlea as compared with the pressure on the lateral part of the trochlea suggests that the distal medial site may be acceptable. It has been proposed that violating an intact joint for the purpose of osteochondral harvest can be associated with marked morbidity, especially in a relatively young patient population. Ahmad et al. described the histological features of the initial graft donor sites of a patient who underwent revision arthroscopy following autologous osteochondral autografting. Examination showed heterogeneous areas of dense fibrous tissue and bone and discrete areas of cartilage. LaPrade and Botker reported on two patients who had donor-site morbidity after an autogenous osteochondral graft procedure. Both patients had fibrocartilage hypertrophy at the donor sites, which contributed to knee pain and occasional locking. A foreign-body giant-cell reaction developed at the donor site in our patient after autologous osteochondral autografting. To the best of our knowledge, this is the first report of a foreign-body giant-cell reaction at the donor site after autologous osteochondral transplant. Granulomatous inflammation is a distinct type of chronic inflammation and is characterized by the accumulation of activated epithelioid macrophages. There are two types of reactions: the nonimmunologic, foreign-body reaction; and the immunologic, hypersensitivity reaction. The foreign-body reaction, composed of macrophages and foreign-body giant cells, is the end-stage response of the inflammation. It consists of macrophages that have been activated by the ingestion of material. These macrophages form multinucleated giant cells that contain foreign material. The undegraded ingested materials induce the macrophage to secrete degradative enzymes, which in turn stimulate blood-borne monocytes to converge around the macrophages and create a granuloma. Foreign-body reaction is a well-known complication following implantation of external devices in the human body. The development of novel biomaterials, biomedical devices, or tissue-engineered constructs necessitates a thorough understanding of the biological responses to implanted materials. Once a biomaterial is introduced into the body, a sequence of events occurs in the surrounding tissue and ultimately ends in the formation of foreign-body giant cells at the tissue-material interface. The consequences of the reaction to the material surface can be devastating. Osteochondral autograft transfer is a relatively safe procedure in that respect, as it involves transferring small osteochondral cylindrical grafts and does not include the use of external devices (i.e., biomaterials) at the implant or donor site. We cannot offer a good explanation for the complication in our patient. Theoretically, no foreign body should have been present as a consequence of this procedure; yet, an ongoing inflammatory reaction directed against a foreign body, with the development of multinucleated foreign-body giant cells, was observed in our patient. It is possible that, at the first arthroscopy, a piece of an instrument remained in the joint, or some material was used to fill the donor site, and this may have caused an inflammatory reaction. However, we were not able to confirm this because the first arthroscopy was performed at another institution and such information was not available in the operative record or from direct questioning of the patient and the original surgeon. Unfortunately, despite our efforts, we were not able to clarify the nature of the material. The slides obtained at the time of arthroscopy were reassessed with the help of a consultant pathologist who had a special interest in musculoskeletal pathology. The histology slides were examined under polarized light, which revealed small shards of birefringent material occupying the empty spaces in the tissue. Not enough material was present, however, to properly identify this material. In conclusion, although osteochondral autograft transfer certainly has a role in the management of osteochondral lesions of the knee, the potential donor-site morbidity and its potential impact on the functional status of the patient have to be taken into consideration when counseling patients about this procedure. Further investigations are necessary to clarify the issue of donor-site morbidity after osteochondral autograft transfer.
Reference: Longo UG, Franceschi F, Ruzzini L, Rabitti C, Maffulli N, Denaro V. Foreign-body giant-cell reaction at the donor site after autologous osteochondral transplant for cartilaginous lesion. A case report. J Bone Joint Surg Am. 2009;91:945-9.
Subacute osteomyelitis at donor site
Giant-cell foreign-body reaction
Inflammatory synovitis at donor site
Pigmented villonodular synovitis


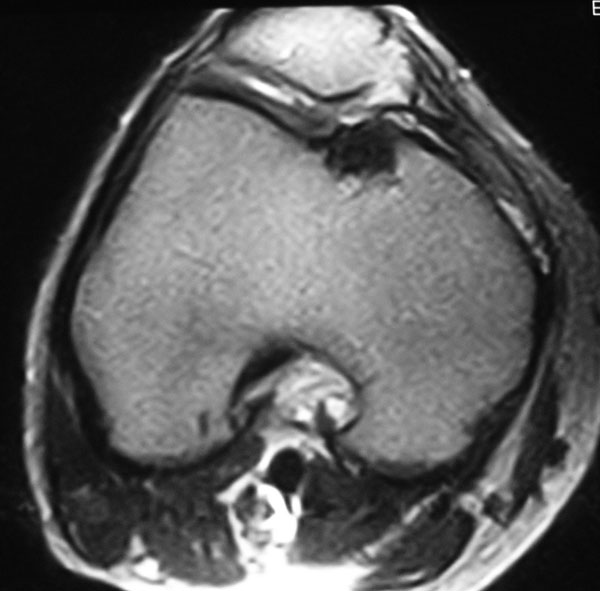
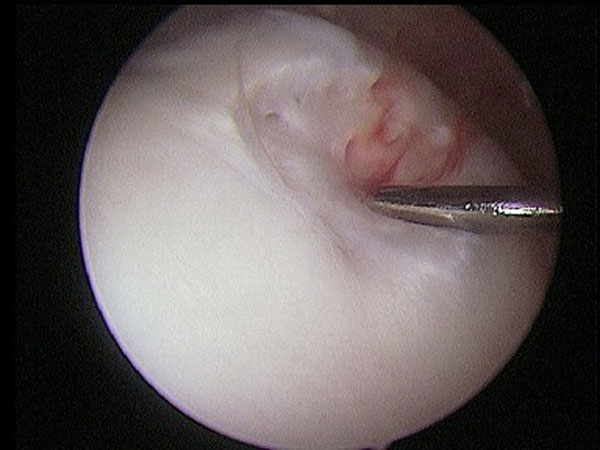
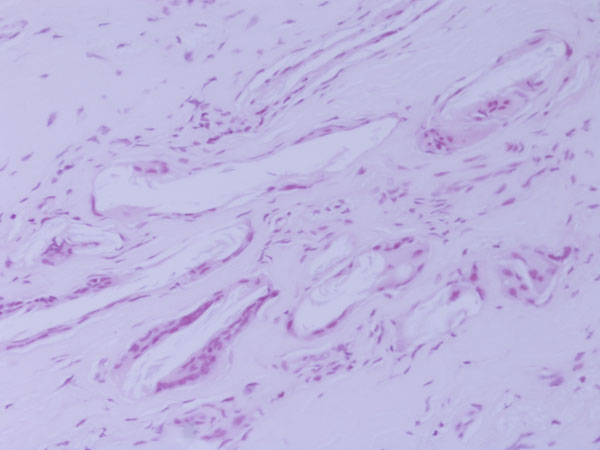
 Fig. 1
Fig. 1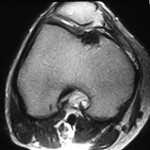 Fig. 2
Fig. 2 Fig. 3
Fig. 3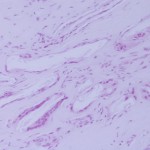 Fig. 4
Fig. 4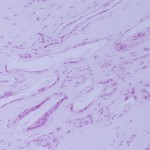 Fig. 4
Fig. 4 Fig. 5
Fig. 5