A Forty-one-Year-Old Man with a Bulging Deformity in the Right Arm
September 3, 2014
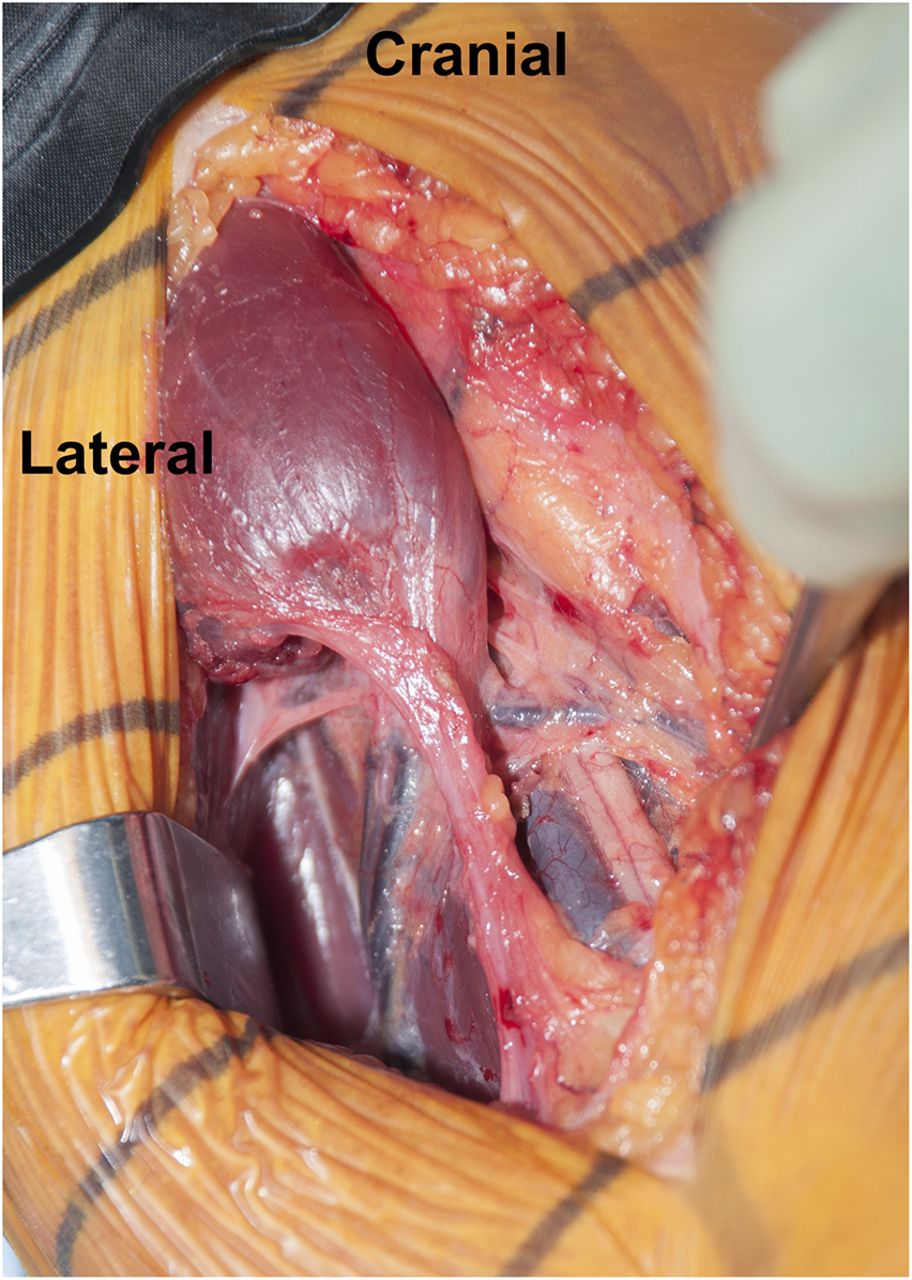
A forty-one-year-old oil rig worker was lifting a heavy piece of equipment by elevating his arm and flexing his elbow when the machine suddenly jerked. He felt a tearing sensation and had substantial pain and deformity in the right arm. Initially, he was seen by an emergency physician, who diagnosed a distal biceps tendon rupture because of the bulging deformity at the medial aspect of the upper arm, as well as weakness and pain during elbow flexion. He did poorly with nonoperative treatment and was referred to an orthopaedic surgeon for consultation. Magnetic resonance imaging (MRI) of the right elbow and the right shoulder was performed; no pathology was evident. The orthopaedic surgeon recommended surgical exploration for diagnosis and potential treatment. Eleven weeks after the original injury, the patient was referred for a second opinion. Examination of the right arm displayed marked deformity and tenderness of the upper arm medial to the biceps (Fig. 1). The patient had no tenderness over the coracoid process or bicipital groove proximally. The biceps tendon was palpable distally, and the hook test was negative. The range of motion of both the elbow and the shoulder was unrestricted. There was weakness in elbow flexion strength, forearm pronation, and shoulder forward elevation (4 of 5 on a scale ranging from 0 to 5, with 5 representing normal strength) compared with the contralateral side. With shoulder abduction, the internal and external rotation strength was normal. The patient showed a mildly decreased sensation at the lateral aspect of the forearm, and he had paresthesia that ran down the forearm whenever he flexed the shoulder or elbow. No additional neurologic deficits were recognized. The imaging studies, including radiographs of the right elbow and MRI of the shoulder and elbow, were normal. Unfortunately, the area of deformity was not included in the previous MRI.
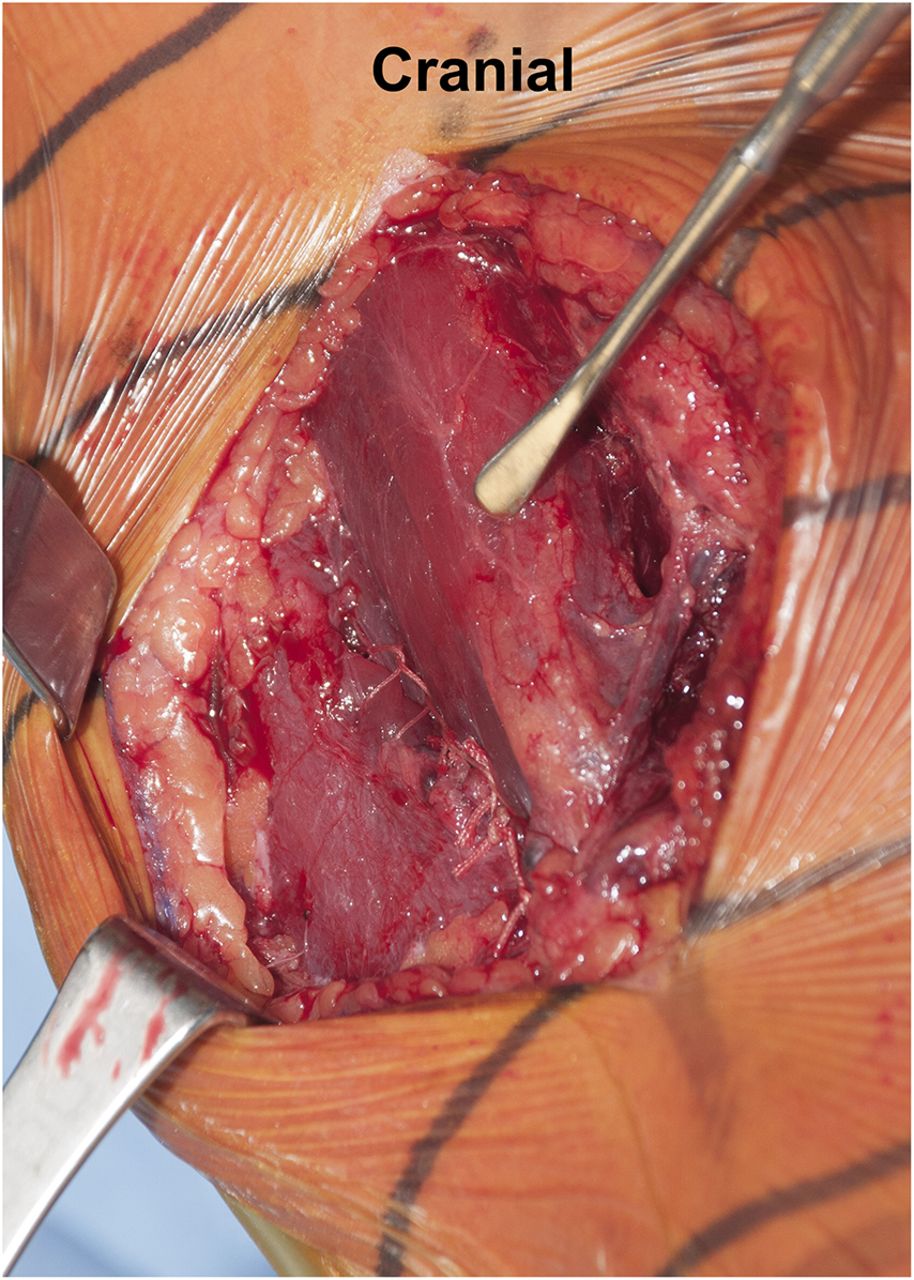
An additional MRI of the upper arm was recommended. This confirmed a distal rupture of the coracobrachialis muscle at the level of the musculotendinous junction (Figs. 2-A and 2-B). Based on the clinical examination and imaging studies, it was concluded that the patient had sustained a distal coracobrachialis rupture, which was causing a traction neuropathy of the musculocutaneous and lateral antebrachial cutaneous nerves. We discussed operative and nonoperative treatment options. The patient elected to proceed with surgical treatment, largely because of the nerve pain and weakness. The goals of surgery were to not only repair the ruptured coracobrachialis muscle, but also to perform a neurolysis of the musculocutaneous nerve to decrease pain, improve elbow flexion and forearm pronation strength, and secondarily eliminate the deformity. Surgical Procedure The patient was placed in the supine position with an attached hand table. A sterile tourniquet was used, and a medial incision was performed through the skin and subcutaneous tissues down to the level of the muscle fascia. The soft tissues were carefully dissected. There was clear disruption with retraction of the distal part of the coracobrachialis muscle (Fig. 3). There was scarring in all tissue planes from the rupture, with a pseudotendon that coursed distally. The muscle-tendon unit was released from the musculocutaneous, lateral antebrachial cutaneous, and median nerves to treat the traction neuropathy, which occurred each time the disrupted muscle fired. The coracobrachialis muscle was then carefully mobilized in order to gain as much muscle length as possible. Because the muscle was considerably retracted, an anatomic reconstruction was not feasible. However, a nonanatomic reconstruction of the retracted muscle was considered because there was no satisfactory location to perform a tenodesis to the bone due to the vicinity of the median nerve, the lateral antebrachial cutaneous nerve, and the brachial artery, and because of concerns about strangulating or entrapping the neurovascular tissues. The coracobrachialis was tenodesed to the adjacent biceps muscle. The only quality tissue was the epimysium. Multiple absorbable sutures (1-0 Vicryl; Ethicon, Somerville, New Jersey) were utilized in figure-eight and modified Mason-Allen configurations to achieve stable attachment to the epimysium. The epimysium was then held in place with a locking suture (2-0 Vicryl) in a Krackow-type locking stitch (Fig. 4). The patient had an uneventful postoperative course and was discharged on the first day with an elbow brace that restricted elbow extension to 90° while allowing full passive elbow flexion. The postoperative regimen began by limiting range of motion to less than 90° of extension; it increased 30° every two weeks by adapting the elbow brace until full extension (0°) was reached at six weeks postoperatively. He was then weaned from the brace and began active flexion of the elbow. Follow-up examinations were performed after two, four, eight, and sixteen weeks. At the last follow-up four months postoperatively, the patient had full range of motion of the right shoulder and elbow. The pain level varied between 0 (at rest) and 5, but had improved from preoperative pain levels. No biceps deformity was present, although some wasting persisted in the area. The neurologic symptoms remained unchanged over the first eight weeks but then improved considerably. The patient reported mild, slightly decreased sensibility of the lateral right forearm at the most recent follow-up. Elbow flexion and forward flexion of the shoulder were improved and back to normal (5 of 5). The patient had resumed full normal activity without pain or discomfort and had returned to work.
Proceed to Discussion >>Reference: Spiegl UJ, Faucett SC, Millett PJ. Traumatic rupture of the coracobrachialis muscle: a case report. JBJS Case Connect, 2014 Jul 09;4(3):e54.
This case report describes the rare case of a distal coracobrachialis muscle rupture caused by indirect trauma. The initial clinical history and examination mimicked a distal biceps rupture, with symptoms including elbow flexion weakness and a bulging area at the medial aspect of the upper arm, which was misdiagnosed as the pathognomonic “Popeye” sign. However, as opposed to the typical distal biceps rupture, which occurs mainly with the elbow extended while lifting heavy objects, this injury occurred with the elbow flexed. On careful examination, the distal part of the biceps was clearly palpable and intact with a normal hook test. The MRI of the right elbow also showed no signs of biceps tendon pathology. Furthermore, the deformity on the medial side of the arm as well as the reduced sensitivity and paresthesia into the lateral lower right arm were atypical. As a result, the correct diagnosis was delayed by over two months. At the time of surgical repair, the muscle was retracted enough that primary repair was no longer feasible. The morphology and variations of the coracobrachialis muscle have been well described in the literature. The coracobrachialis muscle functions as a flexor of the shoulder and is usually pierced by the musculocutaneous nerve. Rupture and retraction of the coracobrachialis muscle can lead to irritation of the musculocutaneous nerve, resulting in weakness of elbow flexion and reduced sensitivity of the lateral forearm, which is innervated by the sensory branch of the musculocutaneous nerve (the lateral antebrachial cutaneous nerve). This is consistent with the operative findings in our patient, which showed considerable scarring and retraction of the muscle to the level of the musculocutaneous nerve, and explains the weakness of elbow flexion and the decreased sensation of the lateral aspect of the lower right arm. In contrast, the decreased forearm pronation strength cannot be explained by the loss of the coracobrachial and biceps muscle function. Since the coracobrachialis muscle rupture occurred proximal to the elbow in our patient, it was not seen on the elbow or shoulder MRI. However, the distal coracobrachialis rupture was visible in the midportion of the humerus on an MRI scan of the upper arm. The delay in treatment could have been avoided with a more careful clinical examination or perhaps by performing an adequate imaging procedure. With earlier diagnosis and earlier surgical intervention, it is conceivable that primary repair of the coracobrachialis back to its anatomic insertion would have been possible. In conclusion, rupture of the distal aspect of the coracobrachial muscle is a very rare injury pattern that occurs after sudden extension and rotation force to the elevated arm. Although the clinical picture may simulate a distal biceps tendon rupture, a negative hook test or reduced sensitivity in the lateral antebrachial cutaneous nerve may indicate an injury of the coracobrachialis muscle.
Reference: Spiegl UJ, Faucett SC, Millett PJ. Traumatic rupture of the coracobrachialis muscle: a case report. JBJS Case Connect, 2014 Jul 09;4(3):e54.
Coracoid fatigue fracture
Musculocutaneous nerve neuropraxia
Coracobrachialis muscle rupture
Medial biceps muscle belly rupture
Brachialis midsubstance muscle tear


 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3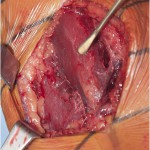 Fig. 4
Fig. 4