An Eighty-five-Year-Old Man with Mild Pain in the Right Knee
August 20, 2014
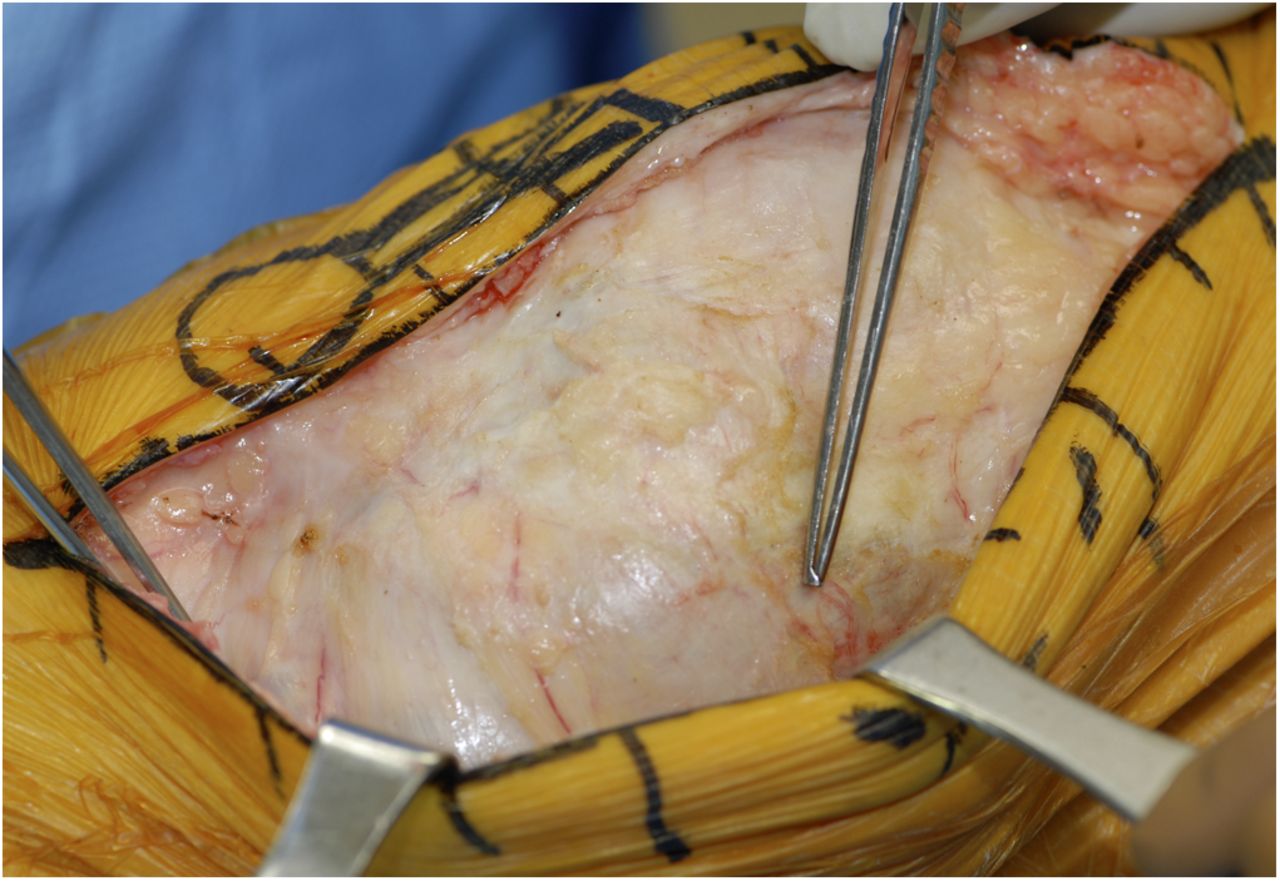
An eighty-five-year-old man presented to the orthopaedic clinic with mild pain on the medial side of the right knee during walking. The patient also noted a small mass over the medial aspect of the knee. Physical examination revealed the mass to be soft, nontender, and mobile. Range-of-motion testing showed a 10° flexion contracture with flexion to 115°. The knee was stable to varus and valgus stress. Radiographs of the knee revealed advanced osteoarthritis of the medial and patellofemoral compartments and a normal appearance of the medial tibial metaphysis. Magnetic resonance imaging (MRI) showed a chronic tear in the anterior cruciate ligament (ACL) and a benign-appearing cystic structure, which extended from the joint line distally along the medial aspect of the proximal tibial metaphysis. Surgical intervention to remove the cyst was discussed, but the patient elected to continue with nonoperative management because the symptoms were well controlled with oral medications. Two years later, the patient noted gradual worsening of the knee pain and enlargement of the cyst. Physical examination revealed a nontender, moderately firm, subcutaneous 8.5 × 5.0-cm mass along the medial aspect of the proximal part of the tibia. The skin overlying the mass was benign in appearance and was freely mobile (Fig. 1). There was no substantial change in the range of motion or stability of the affected knee, and an intact medial collateral ligament (MCL) was noted on valgus stress testing. Radiographs revealed stable patellofemoral degenerative changes with progression of wear in the medial compartment and substantial bone loss in the medial aspect of the proximal tibial metaphysis (Fig. 2). The bone loss was well demarcated and was associated with a sclerotic margin that undercut the articular surface of the medial tibial plateau. The bone loss was thought to represent an erosive pressure phenomenon secondary to the enlarging cyst. Repeat MRI of the knee demonstrated a multilobulated, septated cystic structure arising adjacent to the medial meniscus and extending distally along the medial aspect of the proximal tibial metaphysis (Figs. 3-A, 3-B, and 3-C). The mass measured 8.3 × 4.7 × 3.9 cm and exhibited low signal intensity on T1-weighted images and high signal intensity on T2-weighted images. The majority of the mass was immediately deep to the superficial MCL, which appeared to be intact on MRI.
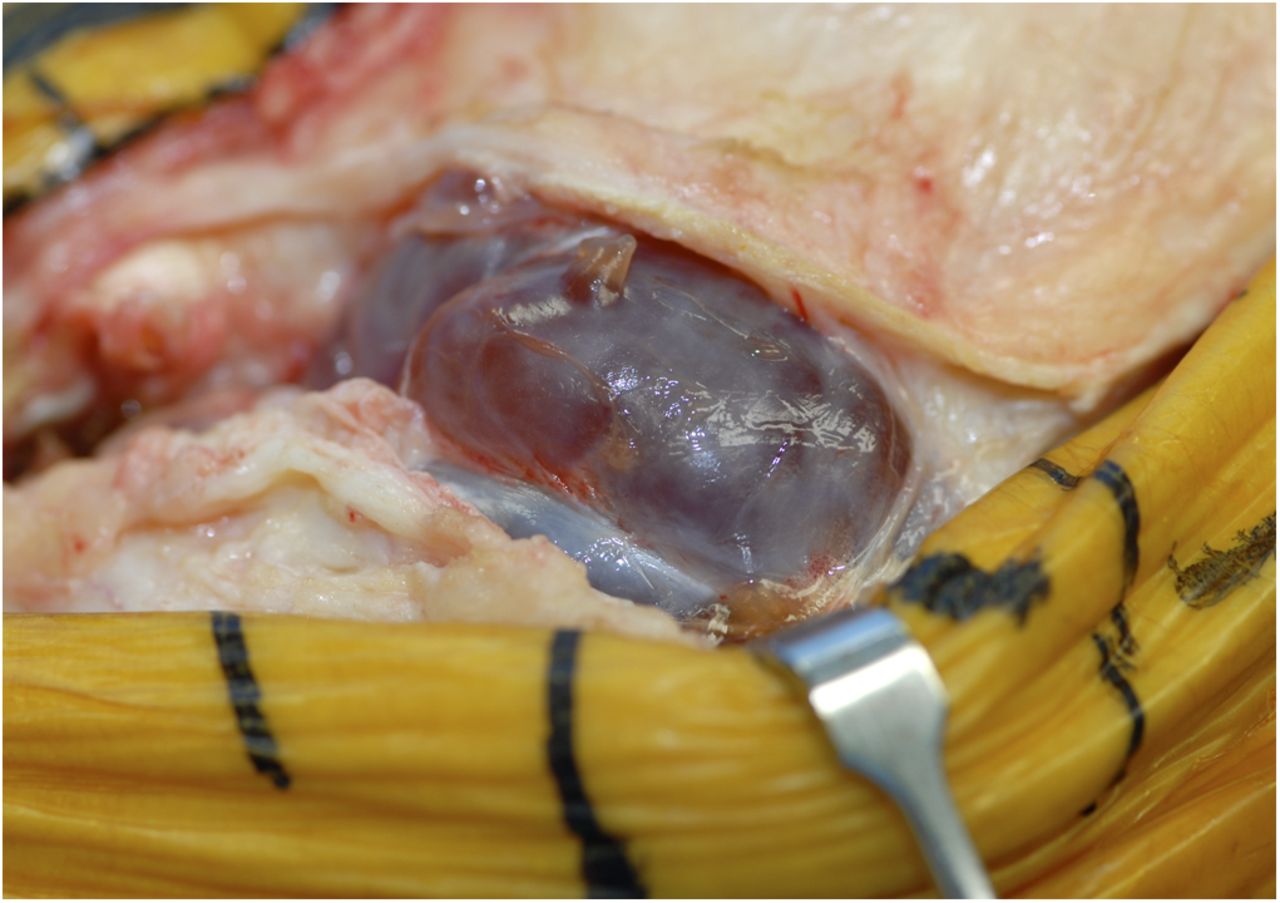
Given the worsening symptoms, the presence of advanced osteoarthritis, and the progressively enlarging cyst with osseous erosion that was believed to compromise the structural integrity of the medial tibial plateau, surgical excision of the cyst combined with total knee arthroplasty with use of a stemmed tibial component was recommended. Intraoperatively, the mass had a thin wall with a distinct tissue plane and contained mucinous material (Figs. 4-A and 4-B). The cyst was excised and was sent for pathological examination. With the cyst excised, the large erosions of the medial aspect of the proximal tibial metaphysis were evident (Fig. 5). The MCL was intact, and reconstruction was performed with a fixed-bearing, posterior cruciate-substituting total knee replacement with a cemented tibial stem extension (P.F.C. Sigma; DePuy, Warsaw, Indiana). The stem length was selected to bypass (and thus offload) the area of erosion, and a cemented stem was selected on the basis of the age of the patient and the quality of the bone. Because the plateau was intact and there was no cortical interruption or substantial loss of cancellous bone, no graft or augment was thought to be necessary. A postoperative anteroposterior radiograph revealed a well-positioned and aligned total knee replacement (Fig. 6-A). Histological examination of the surgical specimen confirmed the benign nature of the cyst, which was determined to be a parameniscal cyst. The postoperative course was uneventful. Routine prophylaxis against deep venous thrombosis (aspirin and mechanical cuffs) and physical therapy were employed. Sixty-seven months after surgery, the patient was walking without the use of an assistive device and had no pain in the treated knee and there was no evidence of cyst recurrence. The Knee Society objective score was 97 points, and the satisfaction score was 40 points. The range of motion of the treated knee was 0° to 112°, and physical examination showed the knee to be stable. An anteroposterior radiograph of the knee that was made at this time (Fig. 6-B) revealed no change in comparison with the immediate postoperative radiograph.
Proceed to Discussion >>Reference: Shin JS, Ou-Yang DC, Gioe TJ. Parameniscal cyst with associated extensive proximal tibial bone erosion: a case report and literature review. JBJS Case Connect, 2014 Jun 11;4(2):e46.
The most popular theory regarding parameniscal cyst development suggests that cysts result from a combination of trauma and degenerative changes that produce a horizontal cleavage tear in the meniscus. Movement of the knee forces synovial fluid into the meniscal tear, and a tortuous tract develops and acts as a one-way valve, preventing the return of synovial fluid to the knee joint. Schuldt and Wolfe found that all fifty parameniscal cysts in their study were associated with a meniscal tear on arthrographic analysis. Similarly, Barrie reported that all 112 excised parameniscal cysts in his study were associated with horizontal cleavage or bucket-handle tears of the menisci. In the latter study, a tract connecting the cyst and the tear was identified in most cases, and fluid from the cysts histologically resembled synovial fluid. Other investigators have contested this theory. For example, Wroblewski reported that only 150 of 299 patients were found to have damaged menisci at the time of surgery. Similarly, Raine and Gonet reported that thirty-six of fifty patients with parameniscal cysts had intact menisci at the time of surgery. Several authors have explained this discrepancy by suggesting that horizontal meniscal tears are not optimally visualized during arthroscopic surgery. More recently, Anderson et al. reviewed 2095 consecutive MRI reports of the knee for evidence of meniscal cysts. A total of 167 meniscal cysts were diagnosed, but only 58% of those were associated with an articular surface tear. The reported prevalence of parameniscal cysts in patients undergoing meniscectomy has ranged from 1% to 22%. Parameniscal cysts are thought to occur two or three times more frequently in men than in women, with lateral cysts being more common than medial cysts by a ratio of 3:1, although Sarimo et al., in a study of thirty-five parameniscal cysts, reported a nearly equal distribution of medial and lateral cysts. Bone erosion secondary to a parameniscal cyst is rare. A MEDLINE search cross-referencing the keywords knee, meniscal cyst, and erosion, and a related search via PubMed, yielded seventeen reported cases. The largest report was the retrospective study by Blair et al., which included seven patients with MRI corroboration. Four of the seven patients had a lateral parameniscal cyst with associated tibial erosion, two had a medial parameniscal cyst with femoral condylar erosion, and one had a lateral parameniscal cyst with femoral condylar erosion. All bone erosions were extra-articular, and all but one involved the margin of the tibia or femur. The exception was a cyst that eroded into the medullary canal of the distal femoral metaphysis. In three cases, radiographs revealed well-defined lesions with sclerotic borders at the margins of the erosions. The remaining ten cysts included seven lateral parameniscal cysts and three medial paramensical cysts. Of the seven lateral cysts, six were associated with erosion of the tibial plateau or femoral condyle and one was associated with erosion of the proximal part of the fibula. Of the three medial cysts, two were associated with erosion of the tibial plateau and one was associated with erosion of the femoral condyle. The diagnosis of a parameniscal cyst is made clinically but may be confirmed with use of MRI. Hallmark symptoms include pain and swelling of the knee, and physical examination often reveals a palpable mass and tenderness along the joint line. Radiographs are usually unremarkable unless bone erosion is present. On MRI, parameniscal cysts classically appear as nonaggressive lesions in the parameniscal tissue that can be unilocular or multilocular and can vary in size. The cyst demonstrates fluid-filled signal characteristics (low signal intensity on T1-weighted images and high signal intensity on T2-weighted images) and may be seen connecting to a meniscal tear. Arthroscopic treatment, including debridement or repair of the meniscal tear and percutaneous decompression or formal resection of the cyst, yields excellent outcomes and low rates of recurrence. Apart from the aforementioned substantial bone erosion and the size of the mass, the parameniscal cyst in the present report had a typical clinical presentation and characteristic MRI findings. As in other reported cases of parameniscal cyst with associated bone erosion, radiographs revealed a well-demarcated, punched-out erosion with a sclerotic margin. To our knowledge, the present report is the first to describe tibial erosion extensive enough to cause concern for the structural integrity of the medial tibial plateau and is also the first to describe treatment with a stemmed total knee implant for this issue. When radiographs reveal well-defined bone erosions with sclerotic margins in the periarticular region of the knee, a parameniscal cyst with secondary bone erosion should be included in the differential diagnosis. For patients with a symptomatic cyst and advanced osteoarthritis, combined cyst excision and total knee arthroplasty can be considered.
Reference: Shin JS, Ou-Yang DC, Gioe TJ. Parameniscal cyst with associated extensive proximal tibial bone erosion: a case report and literature review. JBJS Case Connect, 2014 Jun 11;4(2):e46.
Epidermal inclusion cyst
Arteriovenous fistula
Squamous cell carcinoma
Parameniscal cyst
Synovial cell carcinoma



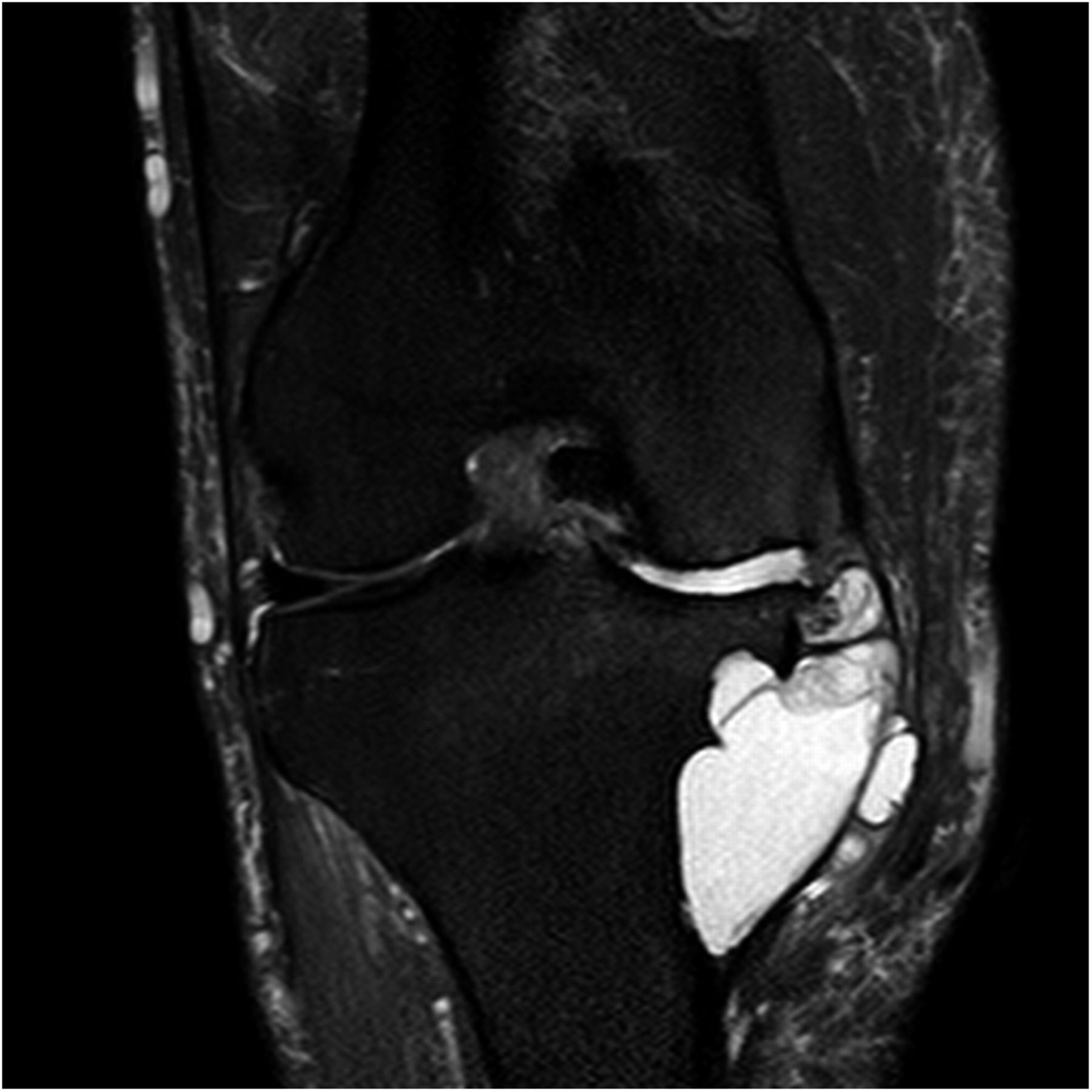


 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3-A
Fig. 3-A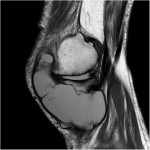 Fig. 3-B
Fig. 3-B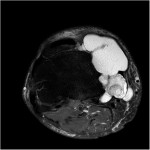 Fig. 3-C
Fig. 3-C Fig. 4-A
Fig. 4-A Fig. 4-B
Fig. 4-B Fig. 5
Fig. 5 Fig. 6-A
Fig. 6-A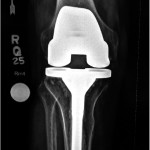 Fig. 6-B
Fig. 6-B