A Thirty-one-Year-Old Man with Acute Right Hip Pain
September 17, 2014
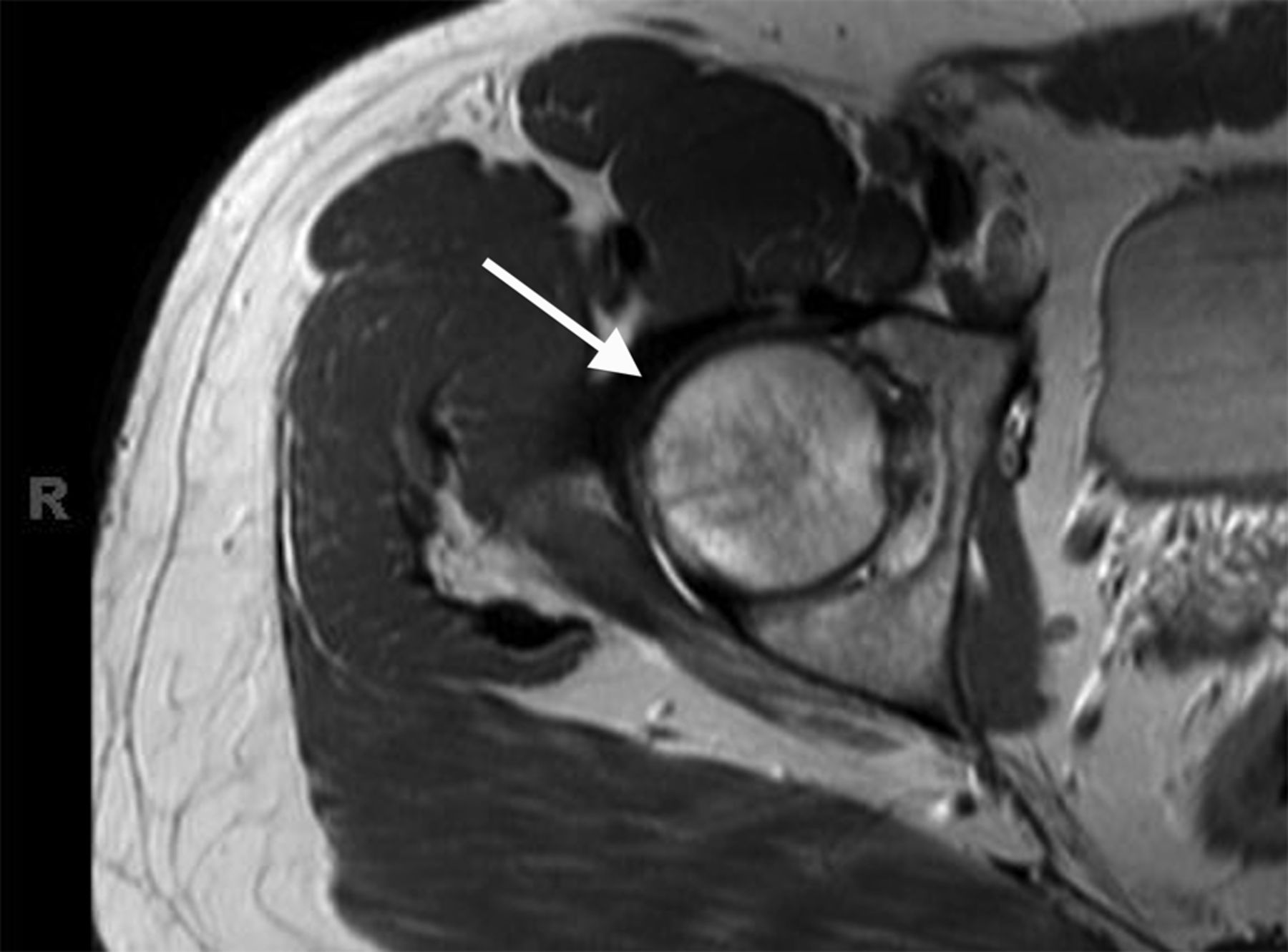
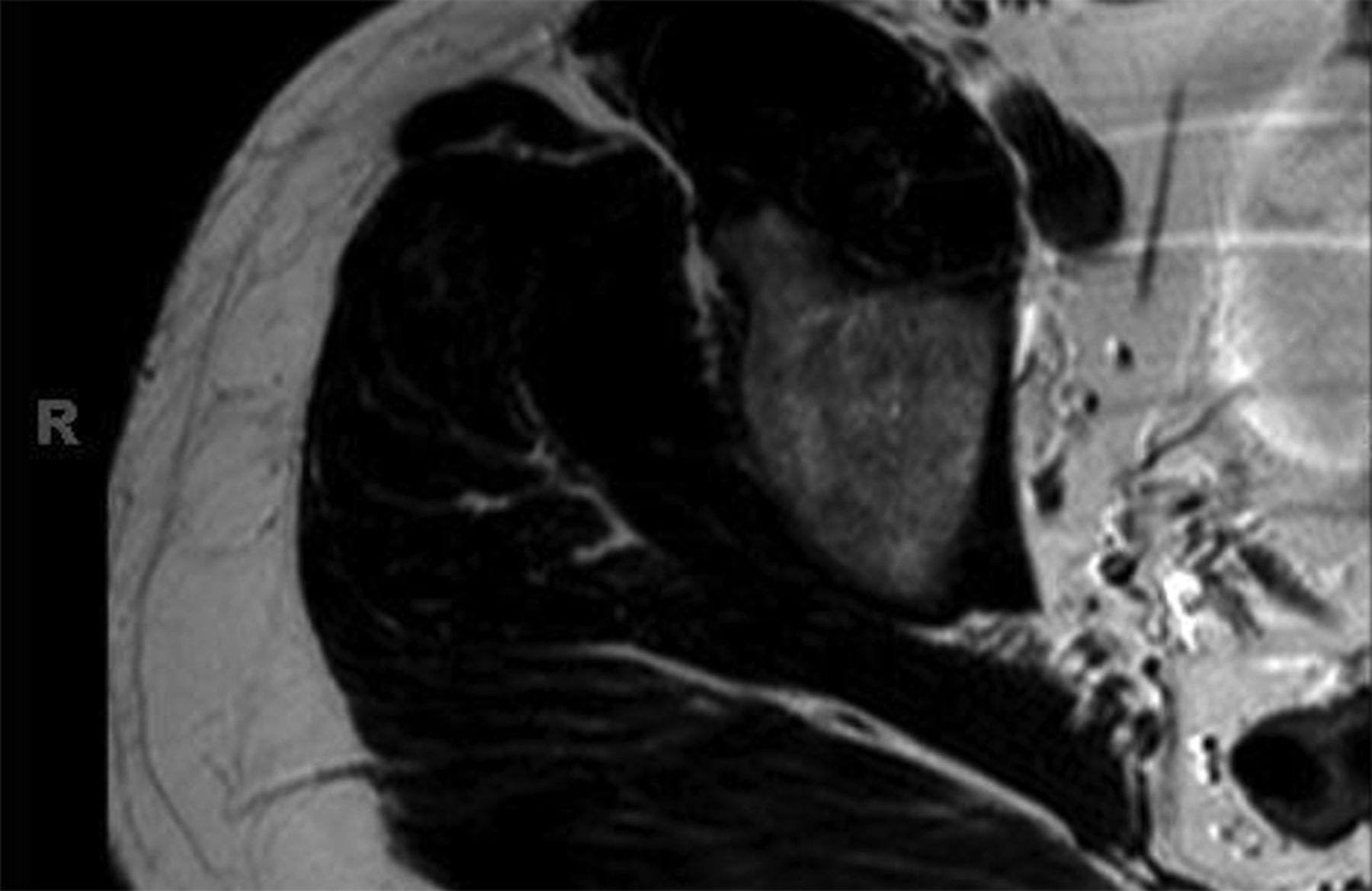
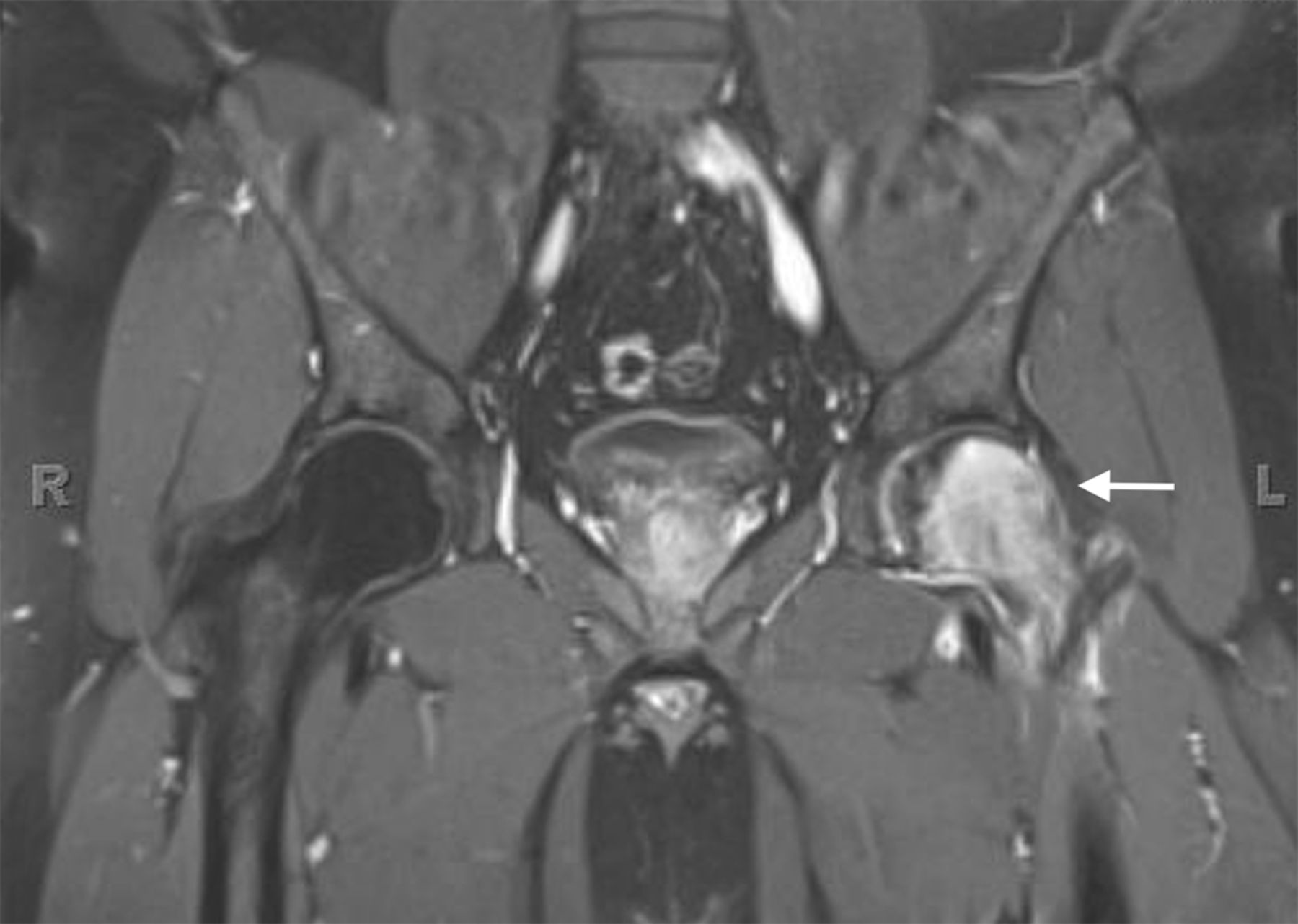
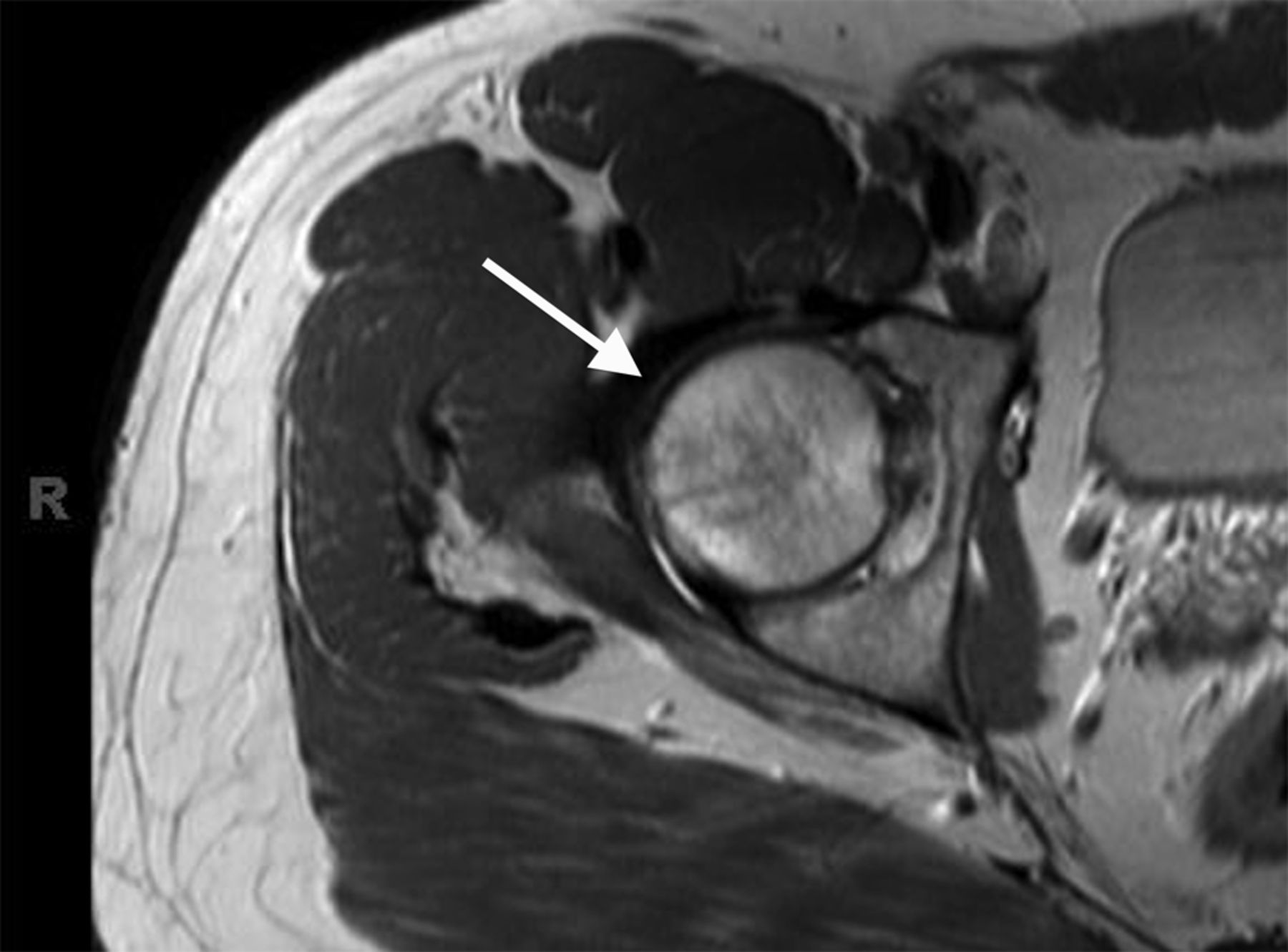
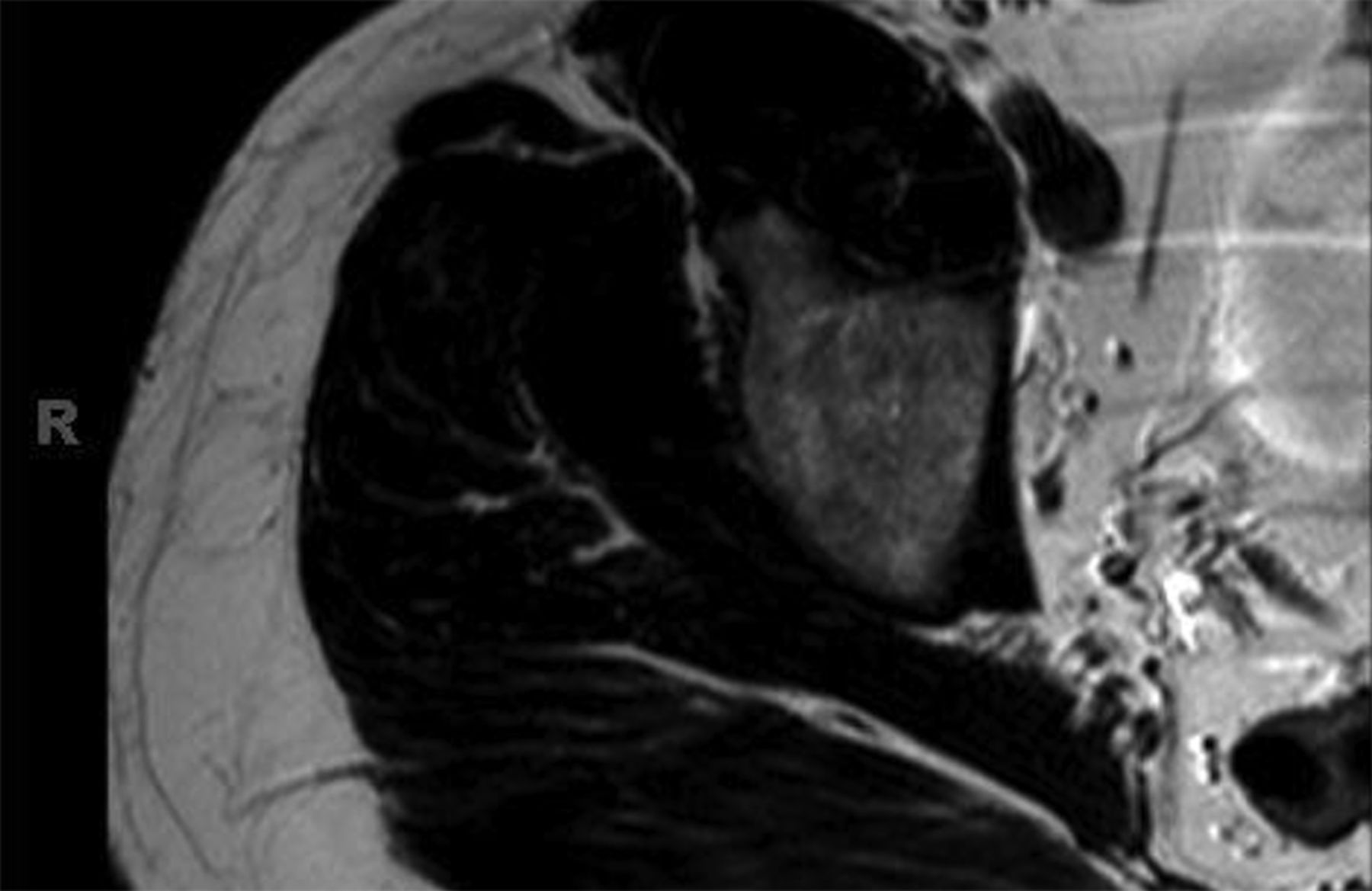
A thirty-one-year-old man developed acute right hip pain that became progressively worse over the span of several weeks. The onset of pain was not associated with trauma, and the patient had no other predisposing factors for osteonecrosis. On physical examination, he demonstrated guarded internal and external rotation of the right hip and walked with a limp; the examination was otherwise normal. Magnetic resonance imaging (MRI) demonstrated decreased T1-weighted signal intensity and increased T2-weighted signal intensity in the right femoral head and neck, consistent with bone marrow edema (Figs. 1-A through 1-D); in Figures 1-B through 1-D, an axial T2-weighted image was used because this study was obtained at an outside institution, and no coronal T2-weighted MRI was obtained.
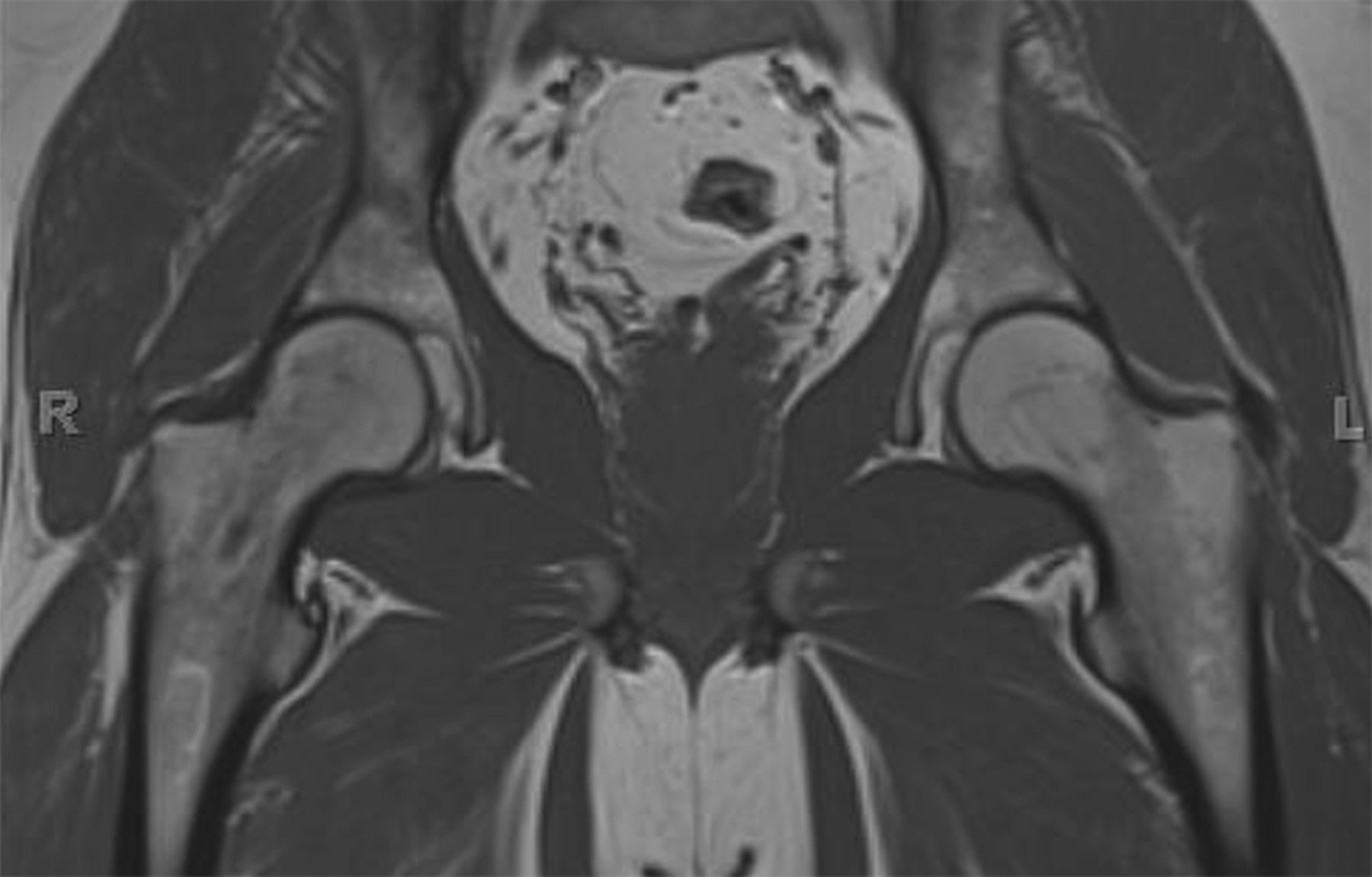
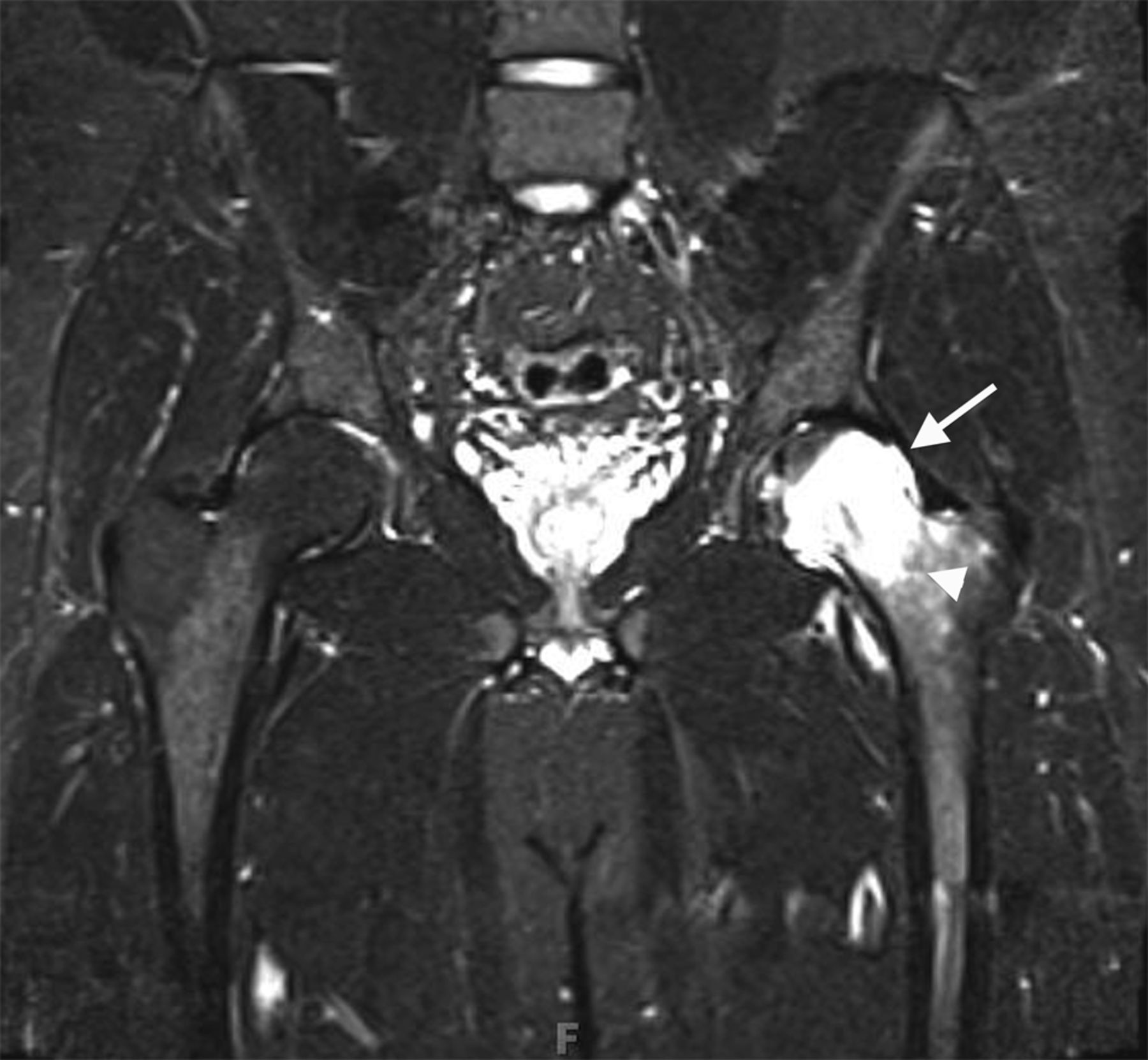
An anteroposterior pelvic radiograph obtained on a subsequent visit demonstrated osteopenia of the femoral head and neck with diffuse cortical thinning (Fig. 2). Because of the worsening clinical presentation and abnormal imaging studies, along with an ongoing concern for underlying neoplasm, a core biopsy of the proximal aspect of the right femur was performed. The biopsy revealed normal bone marrow and no evidence of osteomyelitis, osteonecrosis, fracture, or malignancy. Additionally, the patient was afebrile and had a normal white blood-cell count; a tentative diagnosis of transient osteoporosis of the hip (TOH) was made. Conservative treatment with analgesics and crutches was recommended. Five months later, the patient noted only minor discomfort with prolonged activity. Follow-up MRI demonstrated a return of normal bone marrow signal intensity in the right femoral head and neck (Figs. 3-A and 3-B). A follow-up anteroposterior pelvic radiograph showed remineralization of the proximal aspect of the right femur (Fig. 4). One year after the onset of the right hip symptoms, the patient developed acute left hip pain. He described it as being exactly like the previous right hip symptoms. On physical examination, the patient demonstrated left hip pain with attempted range of motion and weight-bearing; the physical examination was otherwise normal. As before, the patient was afebrile and had a normal white blood-cell count. MRI of the pelvis demonstrated signal abnormalities on short tau inversion recovery (STIR) images indicative of bone marrow edema involving the left femoral head and neck and an associated small joint effusion. Following intravenous administration of a gadolinium-based contrast agent, diffuse marrow enhancement also was present (Figs. 5-A and 5-B); the MRI evaluation of the left hip was performed at our institution, but we used different pulse sequences than those that had been utilized by the outside institution (see Fig. 1). An anteroposterior pelvic radiograph demonstrated osteopenia of the left femoral head and neck (Fig. 6). Conservative treatment with analgesics and protected weight-bearing was recommended. On follow-up six months later, the patient reported that he was doing well and had no pain in the left hip. He declined additional imaging at that time.
Proceed to Discussion >>Reference: Vogler IV J, Caracciolo J, Cheong D. Bilateral transient osteoporosis of the hip: a case report. JBJS Case Connect, 2014 Jul 09;4(3):e56.
The differential diagnosis for young to middle-aged patients presenting with acute unilateral hip pain is broad and can include rheumatoid arthritis, pigmented villonodular synovitis, systemic lupus erythematosus, and acetabular labral tears with or without femoroacetabular impingement. Despite a similar clinical picture, these conditions can be differentiated from TOH by imaging findings. The typical radiographic appearance of TOH is osteopenia of the femoral head and neck without loss of joint space. MRI shows alteration in bone marrow signal intensity involving the proximal part of the femur, with decreased signal intensity on T1-weighted imaging and increased signal intensity on STIR or T2-weighted imaging. These findings are indicative of bone marrow edema. Contrast-enhanced imaging demonstrates diffuse marrow enhancement. A joint effusion is commonly present. Because TOH is a self-limiting condition, radiographs of the affected hip demonstrate remineralization of the proximal part of the femur two to six months following initial presentation. Some conditions, including infection, stress fracture, osteonecrosis, neoplasm, and complex regional pain syndrome (CRPS), warrant special attention because their imaging findings may mimic TOH. When infection occurs in the hip, whether in the form of septic arthritis or hematogenous osteomyelitis, patients usually present with pain, marked limitation in range of motion of the hip, fever, and an elevated white blood-cell count. Despite a similar appearance on MRI studies, differentiating septic arthritis or osteomyelitis from TOH is not difficult on a clinical basis since fever and elevated white blood-cell count are absent in TOH. As septic arthritis progresses, imaging reveals osseous destruction, endosteal scalloping, and subperiosteal reaction, which allows for differentiation from TOH. Patients with stress fractures of the hip typically present with pain brought on by activity, which is relieved by rest. Radiographic features of a stress fracture may include buttressing and sclerosis. On MRI, stress fractures appear as linear zones of low signal intensity on both T1 and T2-weighted images, with surrounding high signal intensity on T2-weighted images; these linear zones are not a feature of TOH. Osteonecrosis characteristically produces pain at rest. Later in the disease process, patients may develop an antalgic gait and limp. Radiographs are typically normal in the early stages of osteonecrosis. In later stages, radiographic findings are often diagnostic with mottled radiolucent areas surrounded by sclerosis. These changes may be followed by subchondral fracture and osseous collapse. MRI findings in early osteonecrosis can mimic those of TOH, with a pattern of bone marrow edema in the femoral head and neck. It is not until the appearance of geographic or bandlike areas of signal abnormality on T1 and T2-weighted images with a “double-line sign” that the diagnosis of osteonecrosis becomes more certain. The clinical presentation of patients with neoplastic disease involving the hip can be quite varied depending on the type of tumor present. Focal areas of bone destruction and/or soft-tissue masses identified on imaging studies differentiate these conditions from TOH. The rounded areas of signal abnormality in the bone marrow of some tumors that are present on MRI are not encountered in TOH. Without findings such as these, however, it may not be possible to separate infiltrative bone marrow neoplasms from TOH based on imaging findings alone. CRPS occurs in patients with a spectrum of conditions. Clinical manifestations include skin abnormalities, edema, and severe burning pain. Pronounced periarticular osteopenia is the typical radiographic appearance. MRI findings may be identical to those in TOH. Biopsies of affected sites reveal lymphocytic perivascular infiltration, edema, and synovial fibrosis, among other changes. Differentiation of CRPS from TOH can be difficult if the characteristic skin changes of CRPS are not present. Recognition of TOH as an unusual cause of acute hip pain may avoid hip aspiration or biopsy in some patients and allow for appropriate therapy. Treatment of TOH in our patient included analgesics for pain control and protected weight-bearing to prevent stress fractures. Other treatment regimens that have been tried with TOH include intra-articular steroid injections, oral steroid therapy, sympathetic blockers, and calcitonin supplementation; none have been shown to be effective at reducing the course of this disease.
Reference: Vogler IV J, Caracciolo J, Cheong D. Bilateral transient osteoporosis of the hip: a case report. JBJS Case Connect, 2014 Jul 09;4(3):e56.
Femoroacetabular impingement
Transient osteopenia of the femoral head
Osteomyelitis of the proximal part of the femur
Hemangioma of the bone
Bone marrow storage disease



![Fig. 1-A Fig. 1-A Coronal T1-weighted (repetition time/echo time [TR/TE], 543/20 msec) non-fat-suppressed MRI of the pelvis and hips showing the bone marrow edema pattern when the patient presented with symptoms. Low signal intensity is observed in the right femoral head and neck (arrow); there is normal marrow signal intensity in the left femoral head and neck.](https://quiz.jbjs.org/wp-content/uploads/2014/09/iqsep14-2_fig1a-150x150.jpg) Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 1-C
Fig. 1-C Fig. 1-D
Fig. 1-D![Fig. 1-A Fig. 1-A Coronal T1-weighted (repetition time/echo time [TR/TE], 543/20 msec) non-fat-suppressed MRI of the pelvis and hips showing the bone marrow edema pattern when the patient presented with symptoms. Low signal intensity is observed in the right femoral head and neck (arrow); there is normal marrow signal intensity in the left femoral head and neck.](https://quiz.jbjs.org/wp-content/uploads/2014/09/iqsep14-2_fig1a-1-150x150.jpg) Fig. 1-A
Fig. 1-A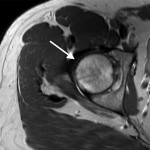 Fig. 1-B
Fig. 1-B Fig. 1-C
Fig. 1-C Fig. 1-D
Fig. 1-D Fig. 2
Fig. 2 Fig. 3-A
Fig. 3-A Fig. 3-B
Fig. 3-B Fig. 4
Fig. 4 Fig. 5-A
Fig. 5-A Fig. 5-B
Fig. 5-B Fig. 6
Fig. 6