A forty-six-year-old woman was seen because of a nine-month history of neck pain. She reported that she had no history of trauma, paresthesia, loss of motor control, bowel or bladder dysfunction, or constitutional symptoms. The pain was exacerbated with flexion and extension movements of the neck as well as during bouts of sneezing or coughing. Anti-inflammatory medications provided minimal pain relief. On physical examination, she could extend the neck only 20° to 30°. Neurological examination showed normal motor and sensory findings, with reflexes bilaterally symmetrical, and a normal gait. Radiographs of the neck showed a lytic lesion that had destroyed the joint between the right lateral masses of the first and second cervical vertebrae and had extended into the second cervical vertebra. A thin sclerotic margin bordered the lesion. No central stenosis was present. Computerized tomographic scans showed invasion of the lesion into the right lateral masses of both the first and second cervical vertebrae. The estimated size of the lesion was 2.5 × 1.5 × 1.0 cm. The lesion also extended into the foramen transversarium of the second cervical vertebra with lateral displacement of the vertebral artery, although the spinal cord was not involved (Fig. 1). An associated soft-tissue mass was noted adjacent to the eroded cortex of the second cervical vertebra. On magnetic resonance imaging, the mass was isointense compared with skeletal muscle on T1-weighted images and mildly hyperintense on T2-weighted images but less intense than cerebrospinal fluid. The overall signal within the lesion was inhomogeneous over several slices on T2-weighted images, and it was enhanced following intravenous administration of gadolinium chelate. The mass was noted to encase the right vertebral artery (Fig. 2). An angiogram showed the flow within the vertebral artery at the second cervical vertebra to be decreased, with its lumen markedly narrowed; however, there was excellent collateral blood flow. On the basis of the radiographic and clinical characteristics, an aneurysmal bone cyst was thought to be the most likely diagnosis. Surgical decompression and stabilization was recommended, but the patient initially refused surgery and was therefore referred for radiation therapy. She received two external beam treatments for a total dose of 400 cGy before an additional review of the magnetic resonance imaging studies indicated that a diagnosis of aneurysmal bone cyst was not certain. A biopsy was recommended. A fluoroscopically guided needle biopsy of the second cervical body was done, but the biopsy tissue was insufficient for diagnosis. The patient finally agreed to an excisional biopsy with possible instrumentation of the cervical spine. During surgery, a combination of posterior approaches was utilized to avoid the need for an additional anterior incision. A far lateral incision was made, with the dissection directed posterior to the sternocleidomastoid muscle. Reflection of the posterior triangle muscles exposed the anterior aspect of the second cervical vertebra. A second incision was made in the midline over the first and second cervical levels exposing the lateral aspect of the first and second cervical vertebrae. A golf-ball-sized, yellow-brown, friable mass was noted to encapsulate the anterior and lateral aspects of the first and second cervical vertebrae. The mass appeared to arise from the right side of the facet joint between the first and second cervical vertebrae. It extended into the lateral mass of the first cervical vertebra and the odontoid process of the second cervical vertebra. Several biopsy specimens were obtained, and the tissue was sent for frozen-section analysis. The diagnosis was deferred pending a review of the permanent sections of the lesion. The remaining mass was curetted from the first and second cervical levels, resulting in a near corpectomy of the second cervical vertebra. The lesion was totally excised. The nondominant right vertebral artery was encased by the lesion and was without a pulse on Doppler-flow testing. The artery was therefore resected. A transarticular screw was then inserted across the degenerative facet between the first and second cervical vertebrae, and autologous iliac-crest bone graft and demineralized bone matrix were packed into the defect after curettage. The graft was secured with spinous process wiring (Fig. 3). The curettage material consisted of multiple fragments of tan-brown and yellow to tan-gray tissue ranging from 0.5 to 2.0 cm in size. Representative sections are shown in Figure 4.
Immunohistochemical staining showed the component cells to be nonreactive for S-100 protein and CD1a. Foam cells, smaller histiocyte-like cells, and giant cells were strongly and diffusely reactive for CD68. Staining for iron showed focal regions that contained abundant iron pigment. The histological diagnosis was pigmented villonodular synovitis. The patient recovered without complications and was asymptomatic two years postoperatively. A computerized tomographic scan showed no evidence of recurrence.
Proceed to Discussion >>Reference: Graham EJ, Kuklo TR, Kyriakos M, Rubin DA, Riew KD. Invasive pigmented villonodular synovitis of the atlantoaxial joint: a case report. J Bone Joint Surg Am. 2002 Oct;84(10):1856-60.
Pigmented villonodular synovitis of the spine is rare, with a cervical location even more unusual. The case of our patient is unique in several aspects. The patient had osseous invasion of the atlantoaxial level that not only thrombosed the vertebral artery but also required extensive curettage that destabilized the spine, necessitating instrumentation and arthrodesis. The present case is the only one, to our knowledge, in which involvement of the first and second cervical levels was clearly documented. The plain radiographic appearance of spinal pigmented villonodular synovitis is variable, but it usually shows destruction of the posterior elements of the vertebral body. The radiographic differential diagnosis includes aneurysmal bone cyst, granulomatous infection, synovial chondromatosis, rheumatoid arthritis, and osteoblastoma. Occasionally, a concomitant soft-tissue mass is present; however, any extradural mass-effect is rarely appreciated on plain radiographs. The features seen on computerized tomography and magnetic resonance imaging in our patient suggested a slow-growing process centered in the synovial joint between the right lateral masses of the first and second cervical vertebrae, with erosion of the adjacent second cervical vertebral body. Pigmented villonodular synovitis of the spine typically arises from the synovial lining of a facet joint. When it is located near a degenerative joint surface, a synovial cyst must be considered in the differential diagnosis; however, pigmented villonodular synovitis may sometimes be differentiated from a synovial cyst on magnetic resonance imaging scans by the localization of areas of attenuation secondary to hemosiderin deposits. The heterogeneous signal of the mass on the T2-weighted magnetic resonance images prompted the reevaluation of our patient. The amount of hemosiderin in the lesion affects its appearance on T2-weighted images. When a large amount of hemosiderin is present, the tumor contains characteristic areas of very low signal intensity on all pulse sequences. However, when there is only a moderate amount of hemosiderin, as in our patient, the intensity of the T2-weighted signal is lower than that usually seen in most soft-tissue neoplasms, but it remains hyperintense compared with that in muscle. Histologically, the lesion lacked the dilated vascular spaces, profuse proliferation of osteoclast-type giant cells, and osteoid-bone formation found in an aneurysmal bone cyst. There was also no evidence of any malignant process. Because of the profuse proliferation of histiocytes, some with clefted nuclei, eosinophilic granuloma was also a histological diagnostic probability. However, the histiocytes lacked the epithelioid appearance of the Langerhans histiocytes, and, immunohistochemically, the cells lacked reactivity for S-100 protein and CD1a, both markers for Langerhans histiocytes. Although pigmented villonodular synovitis may cause focal erosion of bone, especially when arising in a tightly formed joint such as the hip or ankle, extensive bone involvement, as noted radiographically in our patient, is unusual. However, among the cases involving the cervical spine that we are aware of, five of the eight cases that had data from which bone involvement could be determined had such involvement. The preferred treatment of pigmented villonodular synovitis is still complete excision. In our patient, the curettage procedure produced satisfactory clinical results over the two-year postoperative course. With a nearly 100% recurrence rate in the appendicular skeleton following incomplete excision, close follow-up is strongly advocated. Radiation therapy has been proved to shrink the size of pigmented villonodular synovitis lesions, but joint stiffness and local reaction have limited its use in the spine. Radiation synovectomy with yttrium-90 is commonplace in Europe in the treatment of appendicular pigmented villonodular synovitis lesions; however, the potential complications of postradiation malignant tumors, needle-tract necrosis, and severe local reactions as well as the lack of long-term results temper the use of this modality in the treatment of spinal pigmented villonodular synovitis. Radiation as the primary treatment is best reserved for patients who have primary or recurrent disease that is not amenable to operative resection. The choice of operative approach to the body of the first and second cervical vertebrae and the atlantoaxial joint was critical in our patient, as we were able to avoid a transoropharyngeal approach. The posterior approach not only limited the potential morbidity of the procedure but also reduced the total operative time. Treating physicians must consider pigmented villonodular synovitis in the differential diagnosis of destructive lesions of the posterior aspect of the spine, especially when the findings on T2-weighted magnetic resonance imaging suggest inhomogeneity.
Reference: Graham EJ, Kuklo TR, Kyriakos M, Rubin DA, Riew KD. Invasive pigmented villonodular synovitis of the atlantoaxial joint: a case report. J Bone Joint Surg Am. 2002 Oct;84(10):1856-60.
Aneurysmal bone cyst
Pigmented villonodular synovitis
Granulomatous infection
Synovial chondromatosis
Rheumatoid arthritis




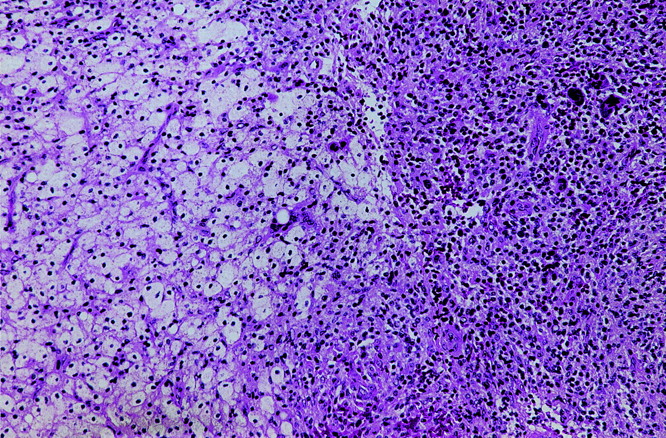
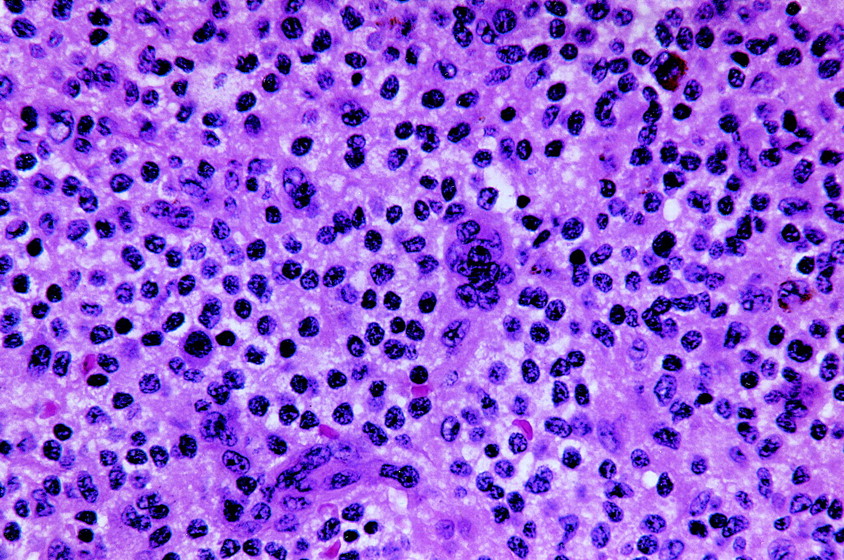
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3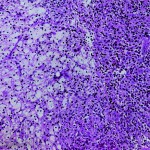 Fig. 4-A
Fig. 4-A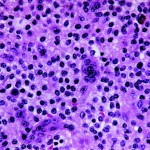 Fig. 4-B
Fig. 4-B