An Eleven-Year-Old Boy with Neck Pain and Torticollis
November 21, 2012
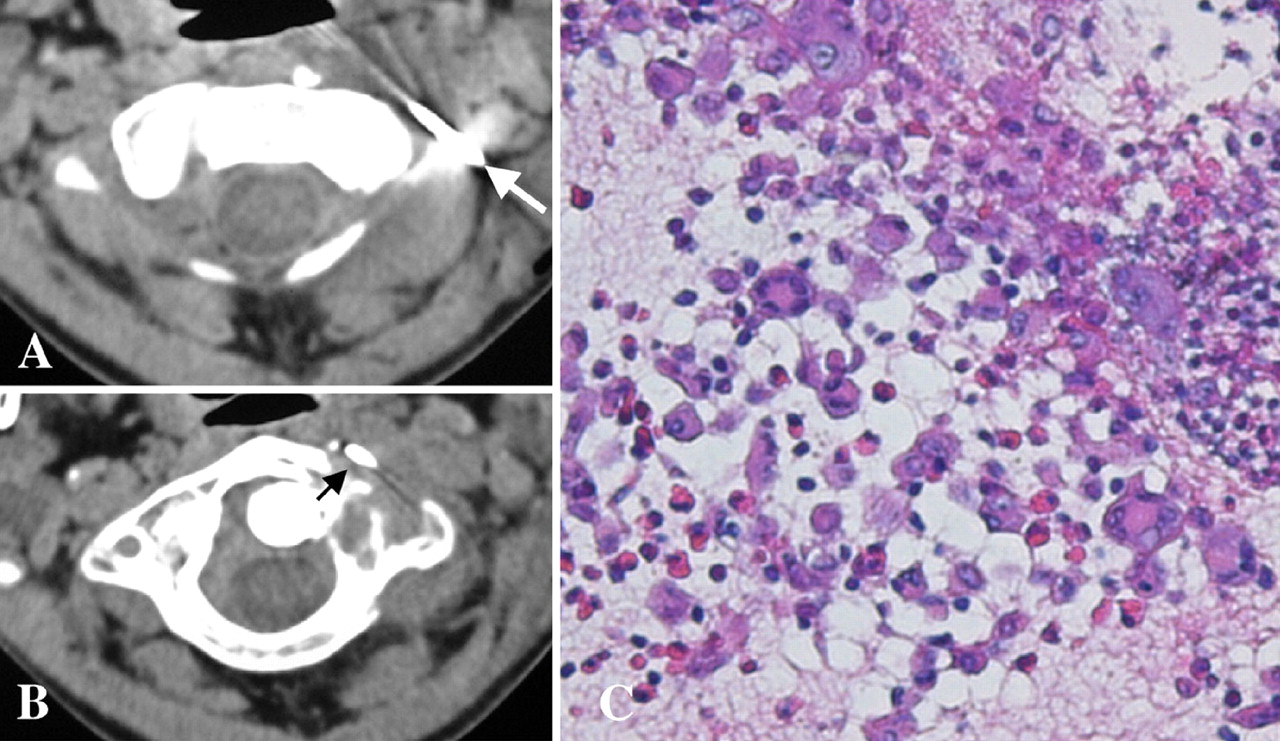
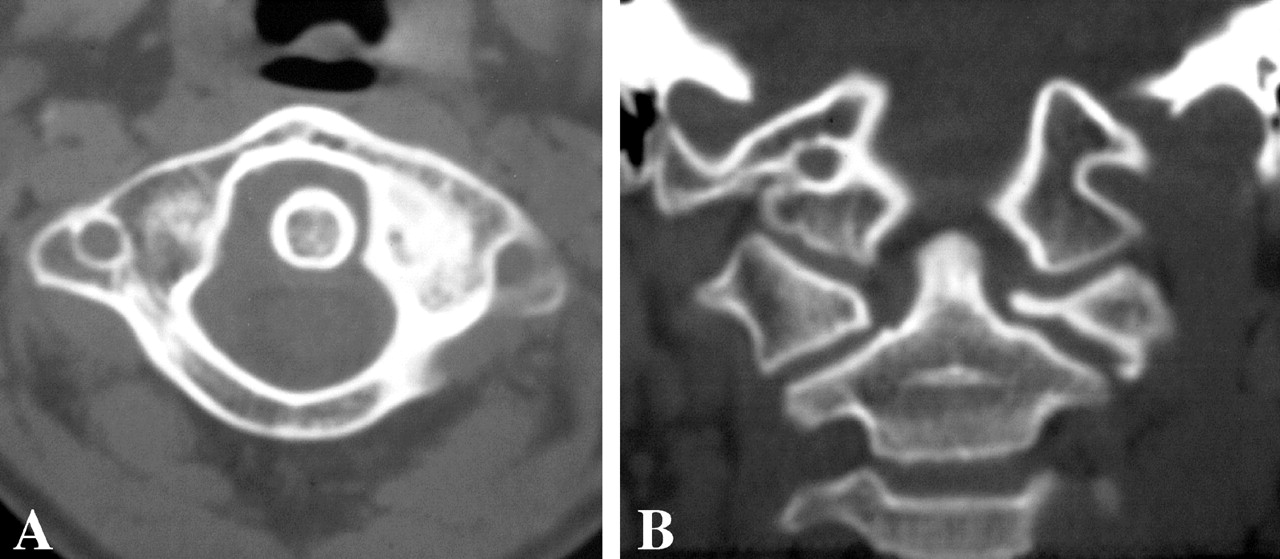
An eleven-year-old boy had neck pain for two weeks followed by the development of persistent torticollis. The neck pain gradually increased, and the symptoms did not improve after the administration of antipyretic drugs. Two weeks after he began treatment, magnetic resonance imaging showed a destructive process within the lateral mass of C1, and the patient was referred to our hospital. The medical history was otherwise unremarkable. Four weeks after the onset of symptoms, the boy required walking aids because of severe neck pain and persistent torticollis; the neck was bent to the left side and slightly rotated to the right side. Physical examination revealed stiffness, pain upon motion of the cervical spine, and tenderness of the left upper cervical spine. There were no neurological deficits. Blood tests showed a slightly increased C-reactive protein level of 0.5 mg/dL (5 mg/L) (normal, 0.0 to 0.4 mg/dL [0 to 4 mg/L]) and alkaline phosphatase of 414 U/L (normal range for an adult, 90 to 340 U/L), while the white blood-cell counts were within the normal range. Cervical radiographs showed torticollis of the cervical spine, and computed tomography demonstrated an osteolytic lesion in the left lateral mass of the atlas (Fig. 1). Magnetic resonance imaging confirmed a mass that was isointensive on the T1-weighted image and high-intensity on the T2-weighted image (Fig. 2). The mass was shown to be expanding to the outside of the atlas on the left side. With the patient under local anesthesia and in a prone position, a percutaneous needle biopsy was performed with computed tomography guidance (Figs. 3-A and 3-B). The biopsy needle was inserted posterolateral to the lesion. There were no complications. A photomicrograph of the biopsy specimen is shown in Figure 3-C.
The histologic findings were diagnostic of Langerhans cell histiocytosis with numerous Langerhans cells and eosinophils (Fig. 3-C). After immobilization of the cervical spine with a collar, the pain and torticollis gradually improved. Low-dose chemotherapy with oral alternate-day prednisone (40 mg per square meter of skin per day) and weekly methotrexate (20 mg per square meter of skin once weekly) was administered for six months, and a cervical collar was worn for four months. No complications accompanied the chemotherapy. The symptoms resolved at twelve weeks, and computed tomography demonstrated partial bone-remodeling. No new symptoms occurred during the follow-up period of twenty-four months, and computed tomography scans made at the latest follow-up examination demonstrated excellent remodeling of the atlas (Fig. 4).
Proceed to Discussion >>Reference: Tanaka N, Fujimoto Y, Okuda T, Nakanishi K, Sumida T, Manabe H, Ochi M. Langerhans cell histiocytosis of the atlas. A report of three cases. J Bone Joint Surg Am. 2005 Oct;87(10):2313-7.
Langerhans cell histiocytosis is a benign condition of localized or multifocal proliferation of histiocytes. Its prevalence is approximately 1:1,500,000 people. Schajowicz reported that 81% of all patients with Langerhans cell histiocytosis have a solitary eosinophilic granuloma, 7% have multiple eosinophilic granulomas, and 11% have widely disseminated lesions of Hand-Schüller-Christian disease syndrome or Letterer-Siwe syndrome. This group of diseases was introduced as histiocytosis X and was later renamed Langerhans cell histiocytosis on the basis of the pathologic findings. Langerhans cell histiocytosis in the spine is relatively rare, with a frequency that has been reported to range between 6.5% and 25%. Clinical symptoms are often severe, and the diagnosis is sometimes difficult. Bertram et al. reported that the cervical spine at C3-C5 is involved in 60% of children with Langerhans cell histiocytosis, but it is quite rare for the disease to affect the atlas. The most common symptoms of Langerhans cell histiocytosis involving the cervical spine are neck pain and restricted range of motion, or torticollis. The three patients described in the present report demonstrated all of these symptoms without neurological deficits. Although lytic lesions of the atlas were found on radiographs, vertebral plana, which is a typical radiographic finding in pediatric patients, was not found. Because the magnetic resonance imaging and computed tomography studies suggested diseases such as osteosarcoma, Ewing sarcoma, and spinal infection, biopsy specimens for histologic diagnosis were required. Computed tomography-guided percutaneous needle biopsies were performed without complications. In our institution, the radiologist does the procedure and frozen sections are made to confirm that the biopsy had obtained lesional tissue. Computed tomography-guided needle biopsy has been reported to be a safe and effective technique for histologic diagnosis, with an accuracy in achieving a diagnosis of 70% to 100%. As for the treatment of Langerhans cell histiocytosis of the cervical spine, many authors have reported that immobilization is adequate for most patients. While an operative procedure may not be needed for a solitary osseous lesion, one of our current patients who had severe torticollis and persistent atlantoaxial subluxation required posterior arthrodesis. On the other hand, Womer et al. described using alternate-day prednisone and weekly methotrexate for the treatment of low-risk Langerhans cell histiocytosis in thirteen patients who were more than one year old and had no bone marrow involvement or organ dysfunction. Twelve of these patients were treated successfully, with limited toxicity manifested by slight and transient elevations in hepatic enzymes in three patients. Those authors concluded that low-dose chemotherapy was safe and effective for patients with low-risk Langerhans cell histiocytosis. The use of chemotherapy to treat Langerhans cell histiocytosis is controversial, but it seems to have been safe and effective in the two patients in the present report who did not have atlantoaxial subluxation. In conclusion, three patients with Langerhans cell histiocytosis of the atlas were treated and all had a full recovery and complete resolution of the symptoms. Imaging studies and computed tomography-guided percutaneous needle biopsies were useful for diagnosing Langerhans cell histiocytosis at an early stage. It is important for surgeons to recognize that Langerhans cell histiocytosis may involve the atlas.
Reference: Tanaka N, Fujimoto Y, Okuda T, Nakanishi K, Sumida T, Manabe H, Ochi M. Langerhans cell histiocytosis of the atlas. A report of three cases. J Bone Joint Surg Am. 2005 Oct;87(10):2313-7.
Aneurysmal bone cyst
Giant cell tumor
Langerhans cell histiocytosis
Fibrous dysplasia


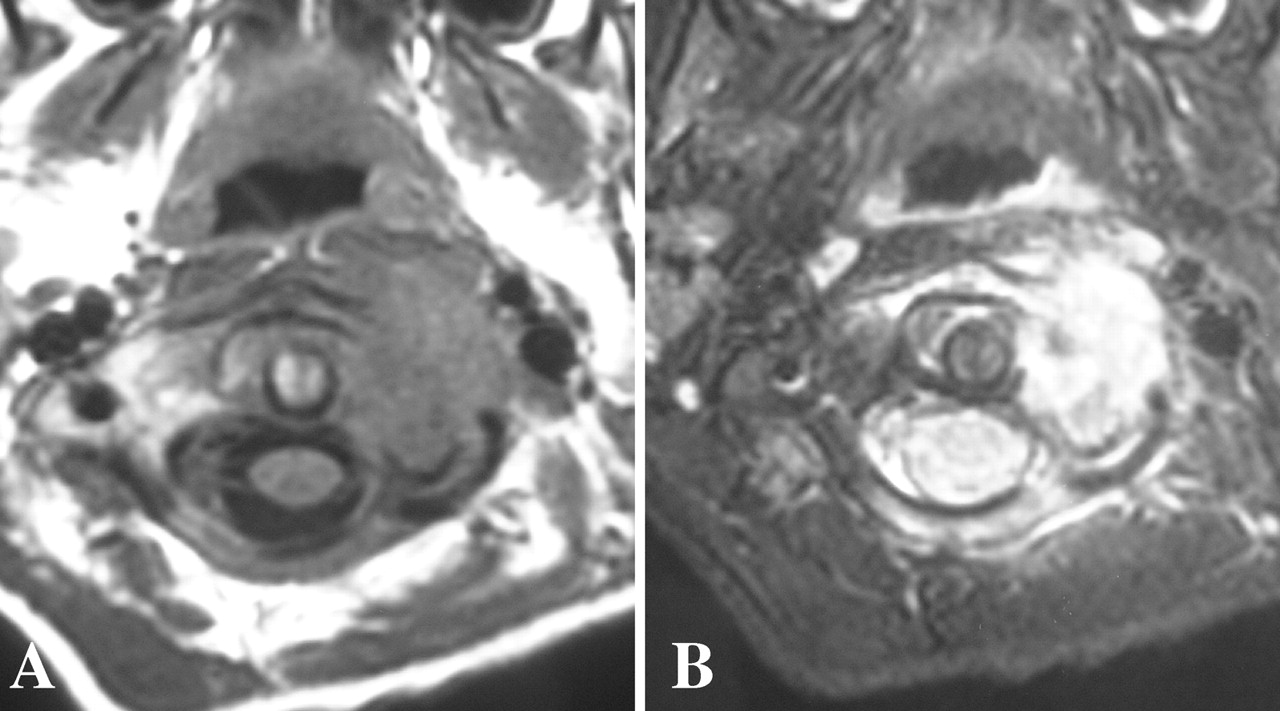
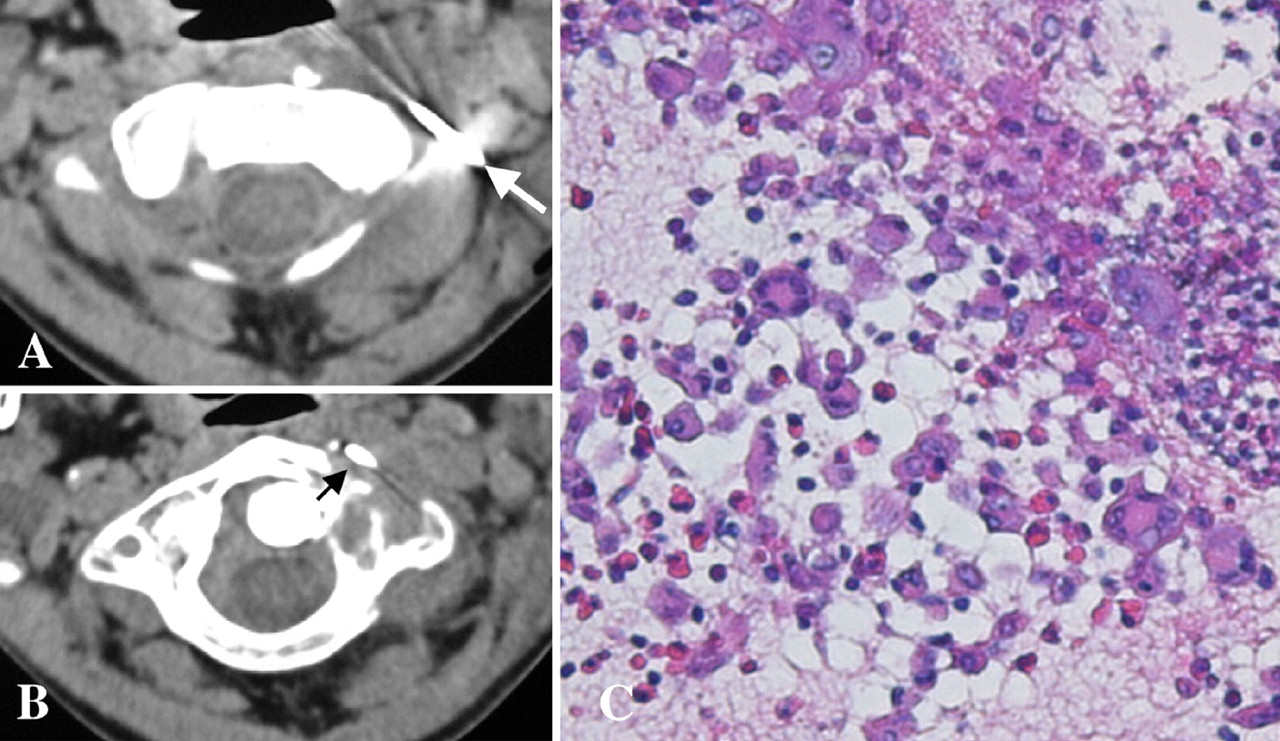
 Fig. 1
Fig. 1 Fig. 2
Fig. 2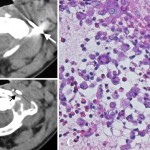 Fig. 3
Fig. 3 Fig. 3
Fig. 3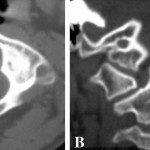 Fig. 4
Fig. 4