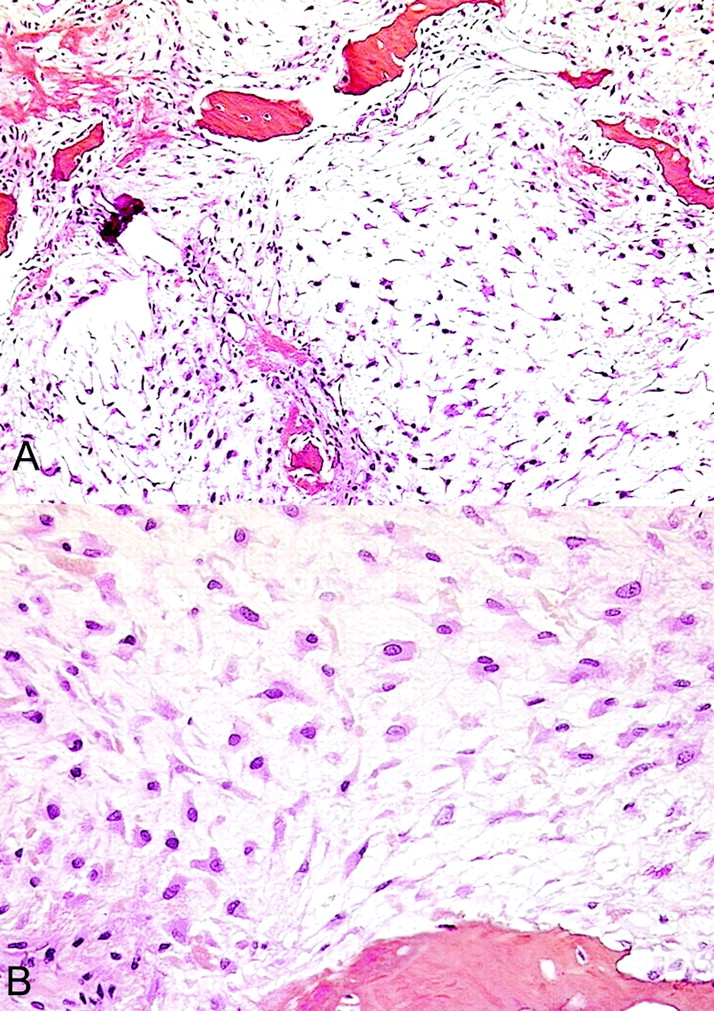
A forty-year-old man was seen in December 2000 with a one-year history of pain in the left hip that had worsened during the previous month. Physical findings were normal except for pain when pressure was applied to the left thigh, distal to the lateral aspect of the greater trochanter. Anteroposterior radiographs revealed a regular, small, lytic lesion, 1 cm in diameter, in the lateral cortex of the proximal part of the femoral shaft (Fig. 1). Computed tomography demonstrated that the lesion was intracortical and well defined and had thin sclerotic margins without medullary or soft-tissue involvement (Fig. 2). Biopsy through a lateral approach showed thickening of the cortex and allowed curettage of the entire abnormal area. Histological features of the biopsy specimen are shown in Figures 3-A and 3-B.
Gross examination of the biopsy specimens showed myxoid and gelatinous tumor material intermixed with a few small foci of hyaline cartilage. Histological features were characteristic of grade-2 myxoid chondrosarcoma (Fig. 3-A). There was a lobulated growth pattern and increased cellularity with spindle-shaped or stellate chondrocytes interspersed in a myxoid stroma without lacunae. The chondrocyte nuclei were enlarged and hyperchromatic, and there were a few binucleate chondrocytes (Fig. 3-B). This proliferating cartilage entrapped and resulted in the resorption of the host bone. A few areas contained hyaline tumor cartilage. Focal necrotic changes were observed. Four weeks after the biopsy, en bloc surgical excision was performed. The lateral aspect of the proximal part of the femoral shaft was reconstructed with allograft and internal fixation. No residual tumor was found on histopathological analysis of the surgical specimen. One year after the operation, the patient was doing well with no evidence of recurrence.
Proceed to Discussion >>Reference: Babinet A, de Pinieux G, Tomeno B, Forest M, Anract P. Intracortical chondrosarcoma. A case report. J Bone Joint Surg Am. 2003 Mar;85(3):533-5.
Chondrosarcomas of bone give rise to some of the most difficult diagnostic and therapeutic problems in orthopaedic oncology. The many anatomic variants described in the literature include central, peripheral, soft-tissue, and secondary chondrosarcomas. Histologically, three unusual forms of chondrosarcoma—mesenchymal, clear cell, and dedifferentiated—that differ in their biological behavior are now recognized. To our knowledge, we are reporting the first case of chondrosarcoma located within the cortex. This chondrosarcoma was myxoid and hyaline, which are the usual characteristics of central and periosteal chondrosarcomas. Usually, conventional chondrosarcomas in long bones grow in a central location. They are usually elongated, well-delineated osteolytic lesions. There is often a fusiform expansion of the shaft with thickening of the cortex. Endosteal scalloping or focal cortical destruction and cortical thickening are characteristic of central chondrosarcoma. Mottled or fuzzy calcifications within the tumor are also characteristic. Spread to the soft tissues is possible but is limited by a pseudocapsule or shell of periosteal new bone. Periosteal chondrosarcomas are more rare and represent only 1% to 2% of all chondrosarcomas. They are delimited by an irregular surface covered by a thick fibrous layer. The soft tissues may be involved. Matrix calcifications are inconsistent findings but are highly suggestive, appearing as spotty, popcorn, or eggshell areas. The cortex may be eroded, saucerized, or thickened. Imaging studies of our patient showed a sharply defined radiolucent lesion consistent with a benign tumor. However, other differential diagnoses of intracortical lesions, such as primary benign neoplasms, non-neoplastic processes, primary sarcomas, and metastases, must be considered in the face of such findings. Most of these lesions can be easily ruled out on the basis of their histological features. The first diagnosis considered for our patient was osteoid osteoma. However, the pain was not worse at night and failed to respond to salicylates, which mitigated against this diagnosis. In addition, no nidus or reactive bone formation was detected on computed tomography. A fibrous cortical defect is usually seen on radiographs as a radiolucent area in the cortex of a tubular bone. The margins are well defined, with a thin rim of sclerosis. The distal part of the femur is the most common site of involvement. There are no clinical manifestations. Intracortical hemangiomas are extremely rare. Most arise in the tibial shaft, although Devaney et al. described a case in the middle of the femoral shaft. Imaging studies may suggest osteoid osteoma or a Brodie abscess. In a minority of cases (three of the nine reported), the lytic variant of intracortical hemangioma exhibits characteristic intracortical calcification of the trabeculae in a vertical alignment. This feature was absent on the plain radiographs and computed tomography scans of our patient. Rudman et al. described an intracortical chondroma of the tibia. The clinical and radiographic features were similar to those in our patient. Intracortical chondroma is extraordinarily uncommon: only one other case, described by Abdelwahab et al., has been reported in the literature, to our knowledge. The diagnosis can be made only on the basis of histological examination. Chondromas do not exhibit extensive myxoid changes or a permeative pattern. Chondromyxoid fibroma is a benign cartilaginous tumor. A few cases arising from the cortex have been reported. Radiographically, however, chondromyxoid fibroma is circumscribed and tends to have a sclerotic border. It is very difficult to diagnose this lesion on the basis of histological analysis because the tumor is easily mistaken for a myxoid chondrosarcoma. Both tumor types have a nodular growth pattern, atypical cells, and myxoid stroma. In chondromyxoid fibroma, however, the lobules are separated by highly cellular fibrous bands containing blood vessels and osteoclast-like giant cells, which is a highly uncommon architecture in chondrosarcoma. Moreover, there is neither bone permeation nor encasement of host bone by the cartilaginous proliferation in chondromyxoid fibroma. Osteomyelitis is considerably more common, and the lesion in our patient was consistent with an abscess. However, there was no history of infection of the femur and no clinical or laboratory evidence of infection. Pronounced sclerosis around the lucency is the rule in infections, but sclerosis was only moderate in our patient. However, many cases of subacute osteomyelitis associated with normal laboratory tests and with features consistent with bone tumor have been described. Thus, the diagnosis of infection can be excluded only by microbiological and histological studies. Aneurysmal bone cyst is a tumor-like lesion. Numerous pathological forms have been described, including cases with a few small cystic lesions confined to the cortex . Internal trabeculations, periosteal reaction, and fluid levels on computed tomography scans are common with this lesion but were absent in our patient. Intracortical osteosarcoma is the rarest form of osteosarcoma. Many cases have been located in the tibial diaphysis. No imaging findings specific to intracortical osteosarcomas have been described in the literature, to our knowledge. Skeletal metastasis is the most common malignant bone tumor. The proximal part of the femur is often involved. Solitary cortical metastasis with no evidence of a primary tumor has been described. The diagnosis can be made by histological examination. In conclusion, intracortical tumors are small well-demarcated lesions that often suggest a benign tumor. Although primary sarcomas such as chondrosarcoma or osteosarcoma account for only a very small proportion of intracortical lesions, the possibility of this diagnosis raises the important clinical issue of how to treat an intracortical lucent lesion. When all of the features characteristic of a benign process are not present, the best course of action is a primary biopsy done through the most direct surgical approach without exposing the neurovascular bundles. En bloc excision is an alternative, but internal fixation or reconstruction is often necessary after cortical resection to avoid fracture. En bloc excision is not necessary for benign tumors and often represents overtreatment.
Reference: Babinet A, de Pinieux G, Tomeno B, Forest M, Anract P. Intracortical chondrosarcoma. A case report. J Bone Joint Surg Am. 2003 Mar;85(3):533-5.
Osteomyelitis
Chondrosarcoma
Fibrous cortical defect
Chondromyxoid fibroma
Intracortical osteosarcoma


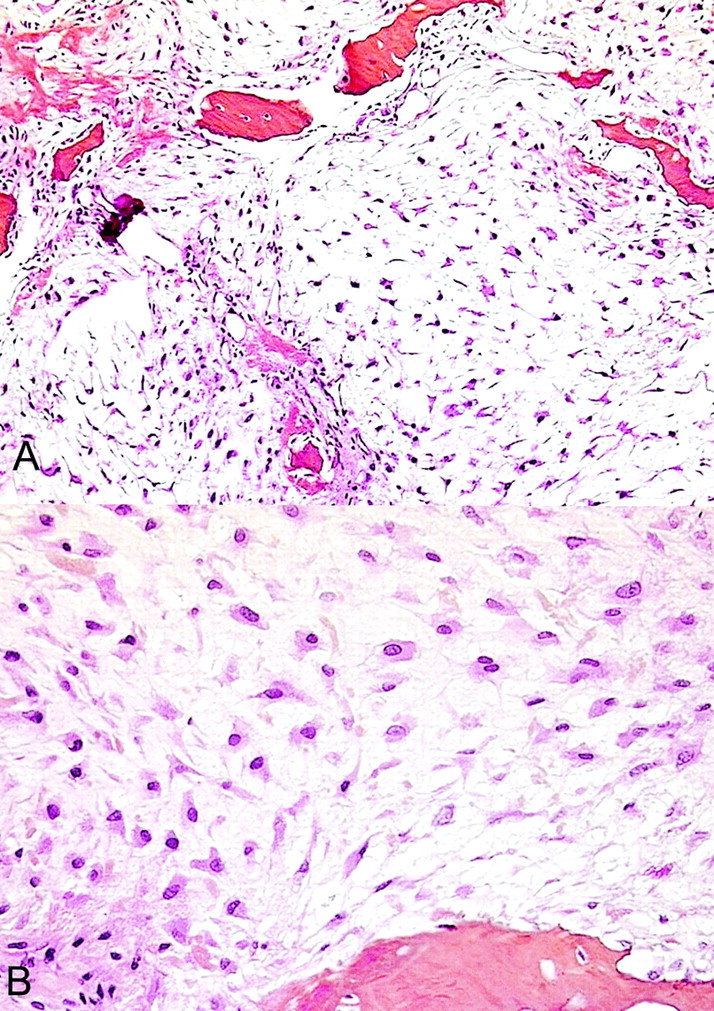
 Fig. 1
Fig. 1 Fig. 2
Fig. 2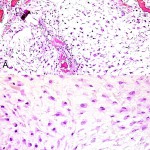 Fig. 3
Fig. 3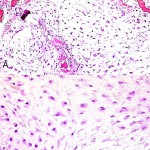 Fig. 3
Fig. 3