While playing outdoor pick-up football, an eleven-year-old boy sustained a left knee injury after being tackled and falling onto the asphalt, landing directly on the anterior aspect of the knee. He was not wearing any protective padding at the time of injury. He developed left thigh and knee pain as well as a large bruise about the thigh and was taken to the local emergency department. He was healthy with no medical problems. On presentation, he had fully intact neurologic and vascular function in the lower extremities and had 5/5 hip and knee flexor and extensor strength despite some pain. He had moderate pain with knee motion, with an active range from 5° to 120° flexion; despite some discomfort, he had a full range of passive motion. The knee was stable to varus and valgus stress, and the Lachman test was negative; additionally, radiographic findings were negative. He was diagnosed with a muscle contusion and discharged with instructions to bear weight as tolerated. Over the next two weeks, the bruising improved but localized about the knee. He had multiple blisters around the anterior aspect of the knee, which eventually opened and drained. He was seen at an outpatient orthopaedic clinic. He had one remaining open blister on the medial aspect of the knee, a nonfluctuant mass in the anteromedial aspect of the knee, and decreased and painful passive knee motion that ranged from 10° to 110° flexion. He continued to be intact from a neurovascular standpoint. He had 5/5 hip flexor and extensor strength but 4/5 knee flexor and extensor strength. A magnetic resonance imaging (MRI) study was obtained (Figs. 1-A, 1-B, and 1-C). The patient was sent to our emergency room for additional management. He reported improving knee discomfort and decreased knee motion, with no systemic symptoms. He walked with a substantial limp, keeping his knee flexed in a position for comfort. On physical examination, he had obvious swelling and ecchymosis about the anteromedial aspect of the knee, which was compressible; blistering and serous drainage were noted around the ecchymotic area (Fig. 2). Passive knee motion ranged from 10° to 100° flexion, limited by moderate pain. In comparison with the contralateral extremity, no gross muscle atrophy was noted. He had 5/5 hip flexor and extensor strength. However, the quadriceps and hamstring muscles were weaker (4/5). He was neurovascularly intact with soft compartments in the leg. Ligamentous examination, limited by discomfort, did not reveal any abnormalities, which was consistent with the MRI findings. The erythrocyte sedimentation rate was 12 mm/hr (normal, 0 to 20 mm/hr), and the C-reactive protein level was 0.5 mg/dL (normal, 0 to 0.9 mg/dL). The white blood-cell count was 9500 (normal, 6500 to 11,000). Blood cultures were negative. Radiographs revealed soft-tissue swelling but no osseous abnormalities (Figs. 3-A, 3-B, and 3-C). Aspiration of the fluid was attempted but was unsuccessful.
The diagnosis of a Morel-Lavallée lesion was made. As the patient reported improved clinical symptoms with no evidence of infection, which was consistent with the reported successful management of these types of lesions about the knees in National Football League athletes, a nonoperative approach was taken. The blisters were dressed with Xeroform (Tyco Healthcare, Quebec City, Canada), the knee was wrapped in a compressive dressing, and the patient began physical therapy focusing on knee motion, stretching, strengthening, and gait training. After three months of follow-up, the patient had no pain and had regained full knee motion and function. At the time of the latest follow-up, six months after the initial presentation, he had no knee pain, had returned to his baseline function, and had 0° to 130° of active knee motion. The visual analog score (VAS) and International Knee Documentation Committee Subjective Knee Evaluation (IKDC) scores were 0 and 100, respectively, indicating no residual limitations.
Proceed to Discussion >>Reference: Anakwenze OA, Trivedi V, Goodman AM, Ganley TJ. Concealed degloving injury (the Morel-Lavallée lesion) in childhood sports. A case report. J Bone Joint Surg Am. 2011;93:e148. doi:10.2106/JBJS.K.00219
Morel-Lavallée lesions (MLLs) are closed degloving injuries that develop as a result of a blunt tangential force that separates the hypodermis from the underlying fascia. The shearing injury to the hemolymphatic supply of the tissue allows the perifascial plane to fill with blood, lymph fluid, and necrotic fat. The hemolymphatic tissue is surrounded by granulation tissue that may be organized into a fibrous pseudocapsule, which prevents resorption of fluid and can lead to clinical presentation in a delayed manner. Reported more commonly in females than in males, this injury can predispose to bacterial colonization and infection because of the static nature of the fluid collection. MLLs have typically been described as occurring along the lateral part of the thigh, buttock, and lower back. More recently, authors have described cases of MLLs involving the knees of football players and wrestlers. The majority of these injuries occurred when the knee struck the playing surface or after an aggressive tackle while the individual was playing football or wrestling. These injuries have been reported mostly in people in their third and fourth decades of life. Our much younger patient was injured during an aggressive tackle while playing football; this mechanism of injury is consistent with cases previously reported in the literature. Although a history of trauma is helpful in directing the clinician to the appropriate diagnosis, the diagnosis of MLL may initially be missed. Hudson et al. reviewed sixteen MLL cases; the diagnosis initially was missed in one-third of the cases. Our patient also was misdiagnosed as having sustained a muscle contusion; he presented to our emergency room with persistent and painful swelling two weeks after sustaining the injury. The rarity of this disease entity in the pediatric population makes the diagnosis more challenging in this age group. A thorough history and physical examination are important to accurately diagnose MLLs in the knee region. Some of the hallmark findings on physical examination include a large and palpable suprapatellar swelling, often extending to the midpart of the thigh medially and laterally, with patchy ecchymosis that can be associated with decreased sensation in the skin overlying the lesion. Because of potential soft-tissue swelling about the knee, cutaneous blisters may be present (as they were in our patient). The differential diagnosis includes ligamentous or osseous injury, muscle sprains, joint infection, and prepatellar bursitis. These can be reliably ruled out by the history, physical examination, imaging studies, and laboratory studies as indicated. MRI studies are the gold standard for diagnosing MLLs and can help in distinguishing MLLs of the knee from prepatellar bursitis, quadriceps muscle contusion, and other common disorders with similar clinical presentation. Therefore, we recommend an MRI when evaluating patients who have sustained trauma to the knee and have physical examination findings similar to those seen in patients with MLLs. Characteristic findings include subcutaneous fluid tracking along the thigh region beyond the area of the prepatellar bursa as well as smooth contours of the fluid collection, which is homogeneously hyperintense on T2-weighted images and hypointense on T1-weighted images. Small globules of fat and lymph may also be seen within the fluid and are highly specific for MLLs in the knee. The treatment goals for patients with knee MLLs are prevention and early resolution of the fluid collection, achievement of full active knee motion, and rapid return to activity. Recent literature has suggested that MLLs about the knee may be successfully treated with simple compression, vasopneumatic cryotherapy, and rest. We employed a similar treatment algorithm for our patient, with the inclusion of physical therapy to promote knee motion and improve gait. If a larger lesion is unresponsive to compression, then drainage may be required. Additional delamination and lesion expansion secondary to contact are a risk with the return to sports activities before complete resolution of the MLL. In refractory cases, talc or doxycycline sclerodesis has been successfully employed. This treatment approach is different from that employed for the more classic presentation of MLL in the pelvic region, which usually follows trauma with substantial pelvic and acetabular fractures. In these settings, optimization of the soft-tissue bed in preparation for surgery to prevent skin breakdown and infection is the main goal. In order to achieve this, evacuation of the fluid collection via open or, as recently described, percutaneous approaches is commonly performed with satisfactory results. In conclusion, MLLs of the knee have become increasingly recognized following injury in contact sports such as wrestling and football and can present a difficult diagnostic dilemma; hence, an MLL must be included in the differential diagnosis of contact-sports athletes, including children, who sustain a shearing knee injury. The MLL, distinct from prepatellar bursitis and quadriceps contusion, is a delamination of the skin and subcutaneous fat from the underlying quadriceps fascia, with rupture of the perforating vessels and the likelihood that large recurrent fluid collections may occur in the space that is potentially created. Nonoperative treatment with early knee flexion and extension exercises remains the most effective means for management of an MLL of the knee. Our case underscores the importance of continued advocacy for safer sports strategies, training, and protective wear during contact sports.
Reference: Anakwenze OA, Trivedi V, Goodman AM, Ganley TJ. Concealed degloving injury (the Morel-Lavallée lesion) in childhood sports. A case report. J Bone Joint Surg Am. 2011;93:e148. doi:10.2106/JBJS.K.00219
Repair of medial patella-femoral ligament
Open irrigation and drainage of fluid collection
Compressive dressing and physical therapy
Percutaneous catheter placement for drainage of fluid collection

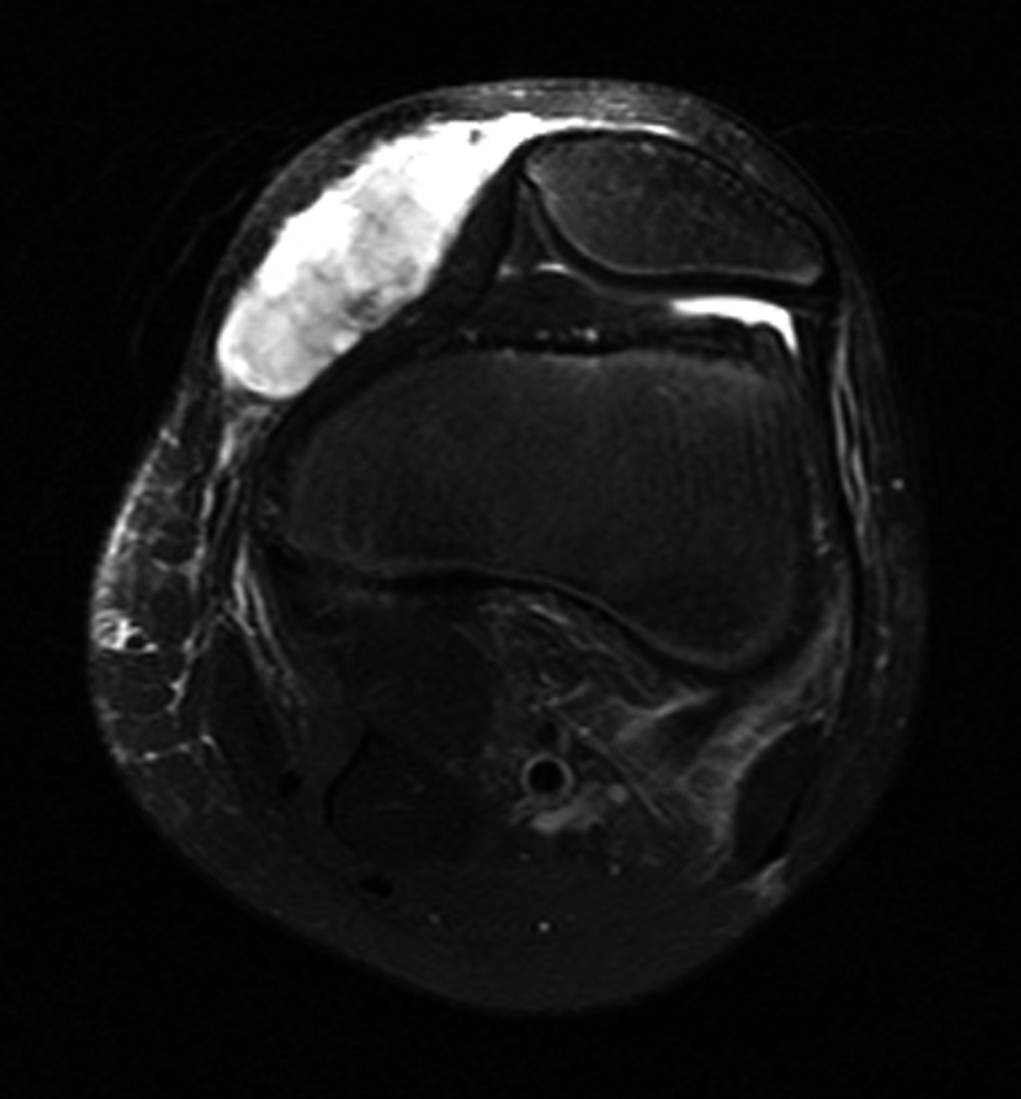
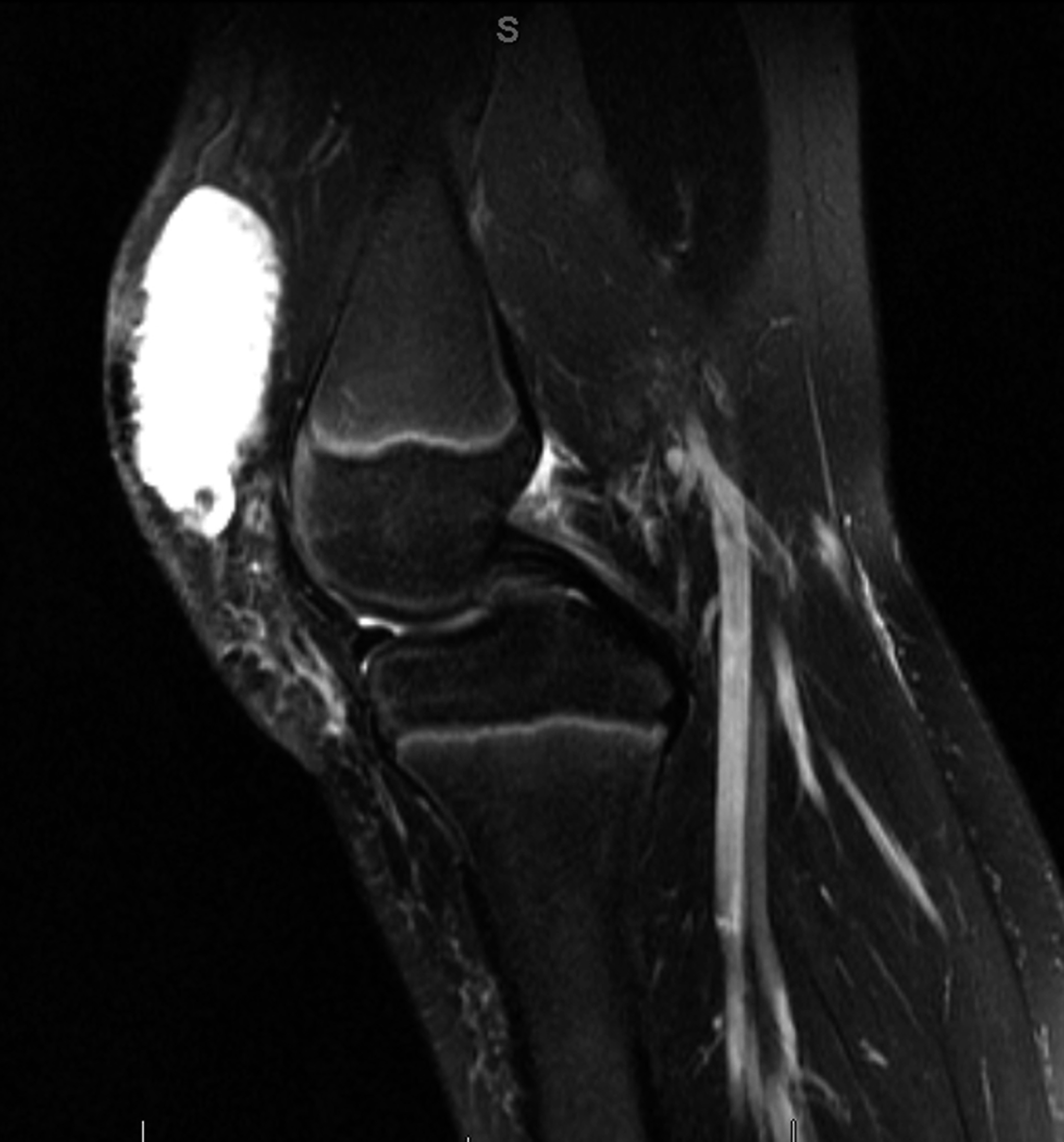
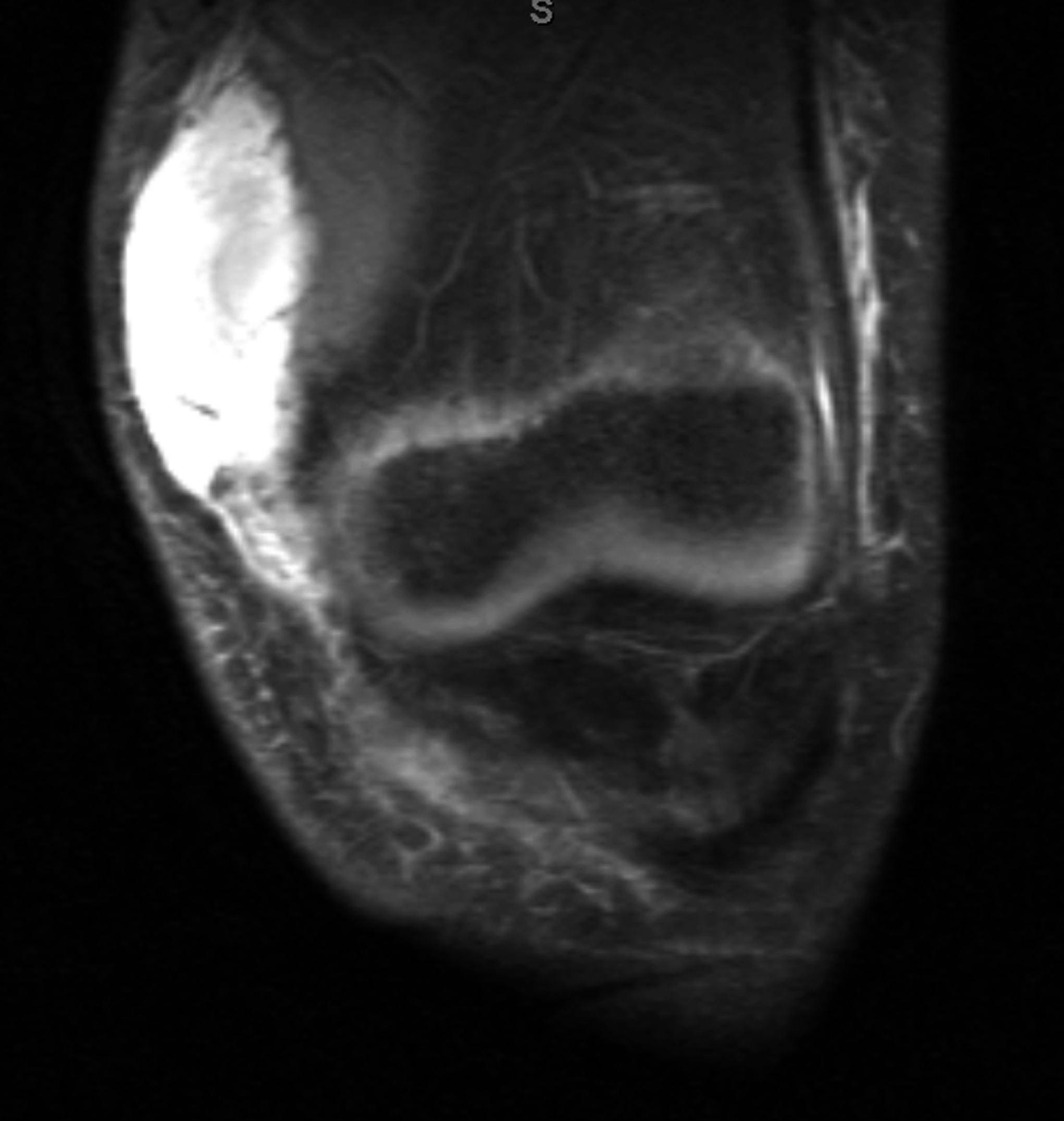


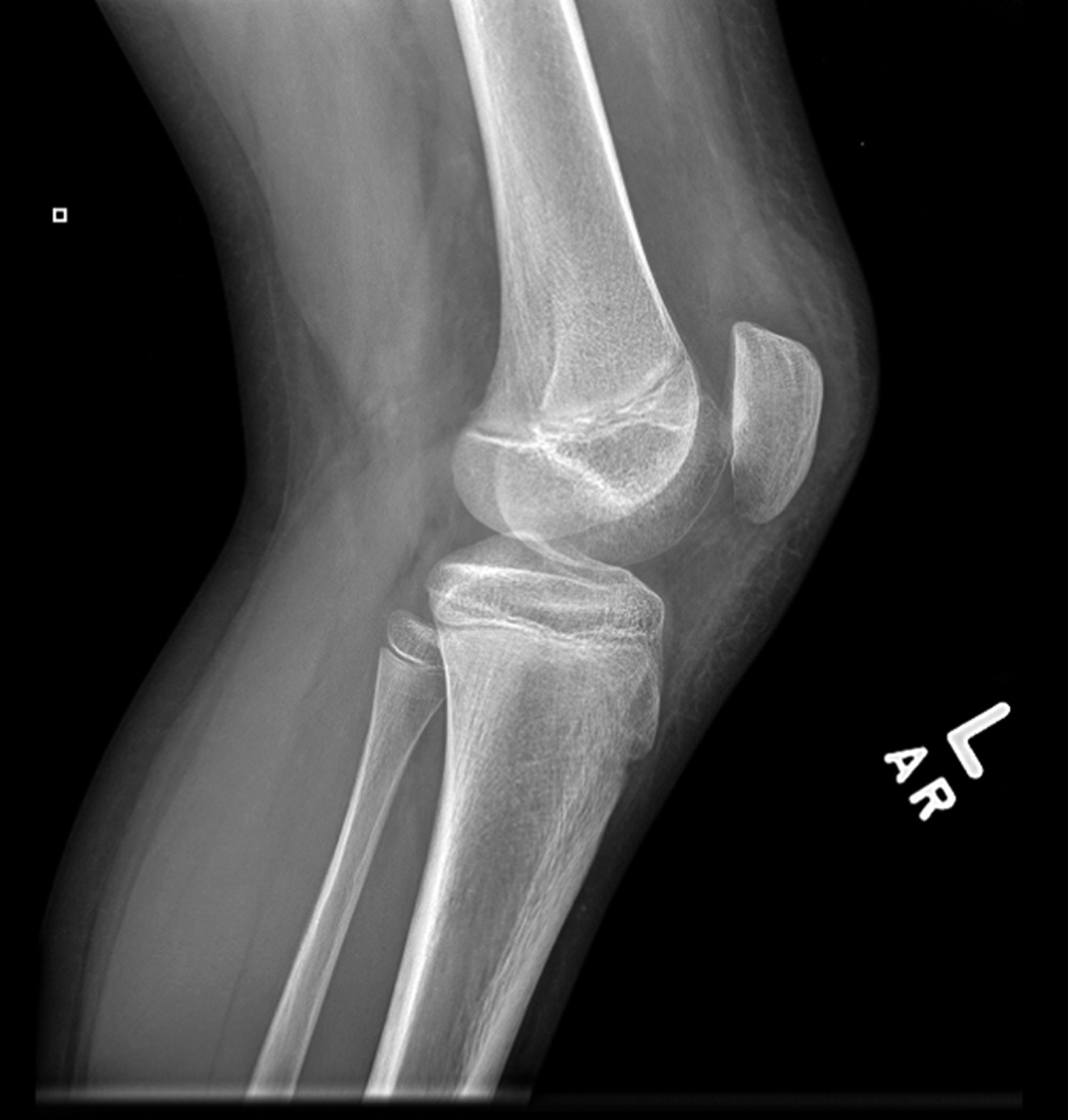
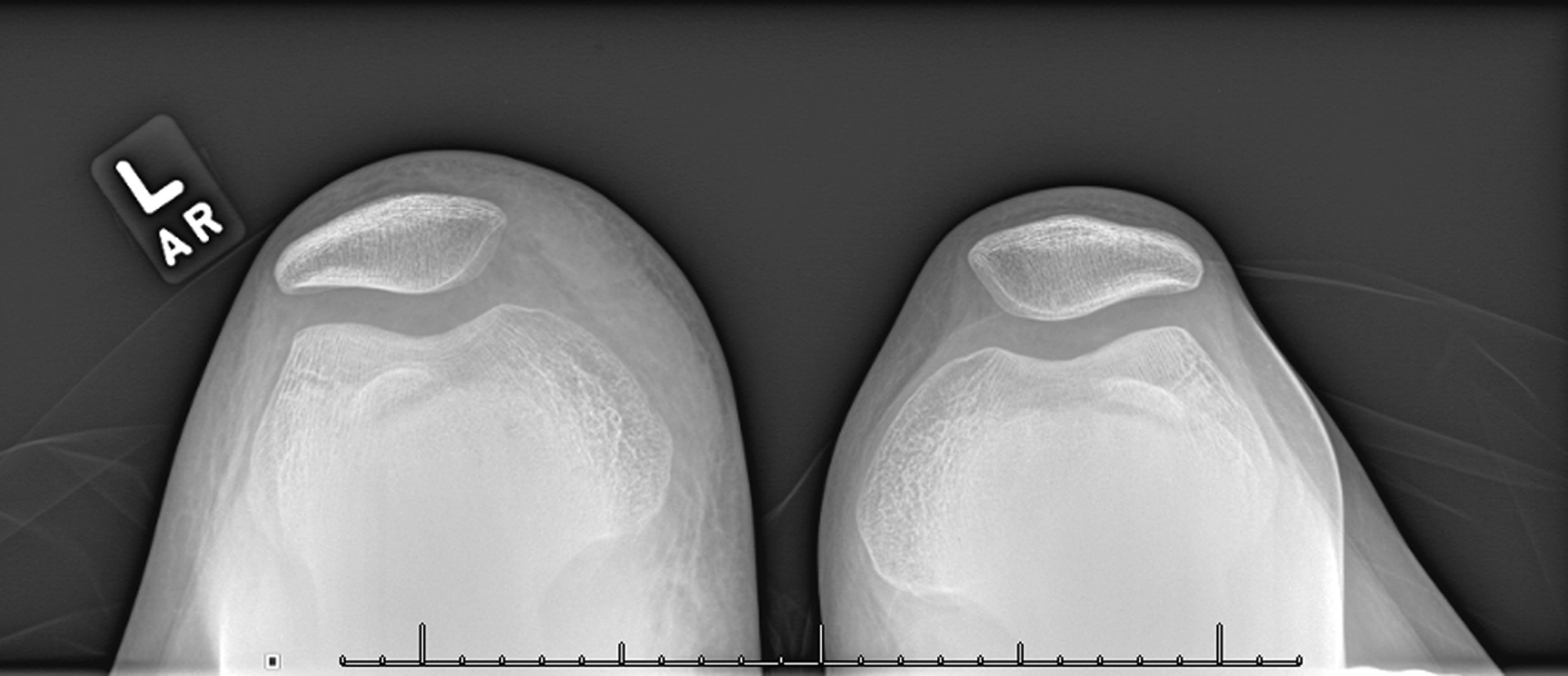
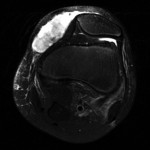 Fig. 1-A
Fig. 1-A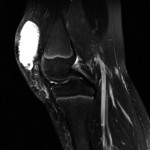 Fig. 1-B
Fig. 1-B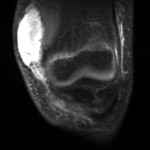 Fig. 1-C
Fig. 1-C Fig. 2
Fig. 2 Fig. 3-A
Fig. 3-A Fig. 3-B
Fig. 3-B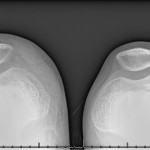 Fig. 3-C
Fig. 3-C