A Fourteen-Year-Old Athlete with Lower-Limb Weakness After a Fall
September 4, 2013
A fourteen-year-old healthy boy presented with an eleven-day history of pain and weakness in the right lower limb. He had developed these symptoms after a fall while jumping and somersaulting during a basketball game. The pain in the right thigh and knee had begun four hours after the incident while he was walking. That same night, he found that he could not stand from a sitting position because of progressive pain and weakness in the injured limb. On the next day, he sought medical help with the chief symptom of pain in the right knee and sacrum. Because radiographs of the sacrum and pelvis revealed normal findings, the patient was prescribed nonsteroidal anti-inflammatory medication and discharged. Ten days later, the patient again sought help for persistent right knee pain, swelling, and lower-limb weakness. He entered the outpatient department with the aid of a wheelchair and could walk only with crutches. He had not experienced back pain or lower-extremity weakness prior to this episode. Physical examination revealed tenderness of the right thigh and patellar tendon, mild swelling of the medial aspect of the right thigh, and numbness of the anterior aspect of the right thigh and medial border of the right leg and foot. Active flexion of the right hip was painful. Active extension of the right knee was lost, and the quadriceps muscle strength was grade 1. Because it appeared that the patient had lumbar radiculopathy with injury of the extension mechanism of the right knee, oral prednisone (5 mg every eight hours) was administered for two days, but the symptoms did not improve. Ultrasonography, performed after the patient had been hospitalized, showed a partial tear of the vastus medialis with active inflammation. Magnetic resonance imaging (MRI) of the lumbar spine was obtained because of the concern for radiculopathy (Fig. 1). The patient’s hemoglobin level was 12.8 g/dL, and coagulation times were normal.
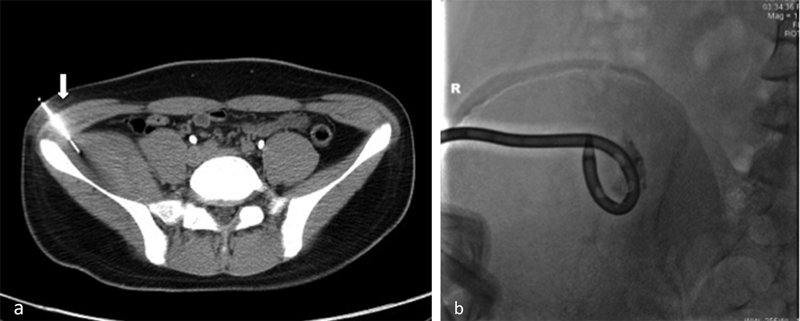
Because of the complete femoral nerve palsy, computed tomography (CT)-guided percutaneous drainage for decompression was performed (Figs. 2-A and 2-B). Initially, 2 mL of blood was drained with a number-14 pigtail tube. This was replaced with a number-16 pigtail tube on the next day, and another 8 mL of blood was drained. The strength of the quadriceps increased to grades 2 and 3 on days two and three after the drainage, respectively. The pigtail tube was retained for three days, and a total of 15 mL of blood was drained. The patient was discharged the day after the drainage tube was removed, and he was able to walk without crutches. Two months later, the strength of the quadriceps was nearly normal. Although terminal extension of the right knee was still lacking and mild numbness was present on the medial aspect of the right leg, the patient became as fully active as he was before the injury. Six months after treatment, the neurologic deficits had completely recovered, and a pelvic CT scan showed a resolved hematoma in the right iliacus with a calcified wall abutting the right iliac bone (Fig. 3).
Proceed to Discussion >>Reference: Kuo HW, Ku JW, Chiang CJ, Rau G, Chen CY, Chen CH. Complete femoral nerve palsy following traumatic iliacus hematoma: a case report and literature review. JBJS Case Connector. 2013 Jul 24;3(3):e74.
Most retroperitoneal hemorrhages, including iliacus hematoma, occur in patients with hemophilia and in those receiving heparin or oral anticoagulants; they also occur following spontaneous bleeding, minor trauma, hip or pelvic orthopaedic surgeries, and abdominal surgeries. The incidence of retroperitoneal hemorrhage is reportedly 1.3% to 6.6% in patients who use antiplatelet agents, and 5.5% to 10.4% in patients with hemophilia. Iliacus hematoma causing femoral nerve symptoms after trauma in healthy individuals is rare. In our case, the mechanism of injury was suspected to be a blow to the back after a fall while somersaulting. The reported treatments of iliacus hematoma include conservative management, transarterial embolization, percutaneous decompression, and surgical decompression. Because femoral neuropathy secondary to an expansive lesion in the psoas may result in increased iliacus compartment pressure and femoral nerve compression or ischemia, the aim of treatment in the acute phase is to stop additional bleeding, relieve pain, and reduce neural damage. However, the treatment of iliacus hematoma associated with femoral neuropathy remains controversial because of the rarity of this condition. Additionally, the patient’s age, comorbidities, and causes of bleeding may affect the therapeutic outcomes. Patients with coagulopathy experience bleeding tendency and comorbidities that may alter the recovery of femoral nerve function. Thus, surgical hematoma evacuation has been highly recommended in patients with coagulopathy because permanent neuropathy can occur following conservative treatment. In contrast, fourteen case reports of seventeen previously healthy patients with traumatic iliacus hematoma showed excellent results in seven patients (41%) with incomplete femoral neuropathy. Five patients underwent nonsurgical treatment and two underwent surgical decompression; they all recovered completely. Ten (59%) of the seventeen patients had complete femoral neuropathy; nine of these patients underwent surgical hematoma evacuation, and only one of the nine had residual neuropathy. Only one patient with complete femoral neuropathy underwent nonsurgical treatment and had residual neuropathy at the one-year follow-up. In the present case, the patient had complete femoral neuropathy and underwent CT-guided percutaneous decompression fourteen days after the injury, resulting in drainage of 15 mL of blood in three days and increased strength of the quadriceps to grade 3. He returned to full activity seven weeks after treatment and showed complete recovery six months later. After the decompression, the complete palsy became incomplete palsy, and it then resolved spontaneously. Although a partially organized hematoma is difficult to drain, a larger-sized drainage tube and sufficient drained volume to improve neurologic symptoms may achieve the goal of treatment in patients with complete femoral nerve palsy secondary to traumatic iliacus hematoma. Diagnosis of femoral neuropathy is difficult not only because of its rarity but also because it mimics lumbar radiculopathy. The femoral nerve is formed by the three posterior divisions of the second, third, and fourth lumbar (L4) nerves. The sensory distribution of the femoral nerve consists of the anterior aspect of the thigh and medial border of the lower leg, although the dermatome of the L4 nerve extends from the anterior aspect of the knee to the medial malleolus. The quadriceps femoris shows weakness in both femoral neuropathy and L4 radiculopathy, whereas the iliopsoas shows weakness in femoral neuropathy but shows normal strength in L4 radiculopathy. In previous reports, all of the patients described weakness or palsy of the quadriceps femoris and pain during hip flexion; additionally, they all had sensory loss over the anterior aspect of the thigh, but only a few mentioned numbness of the medial aspect of the lower leg. Our patient described pain during active hip flexion and loss of knee extension. Numbness was located from the anterior aspect of the thigh to the medial border of the lower leg and foot. Although the musculoskeletal sonograph showed a partial tear of the vastus medialis, and the MRI of the lumbar spine showed bulging disc at the L4-L5 level, the initial clinical impression was incorrect. Fortunately, the terminal MRI showed a large iliacus hematoma with femoral nerve compression, enabling accurate diagnosis. In conclusion, femoral neuropathy may mimic lumbar radiculopathy and should be differentiated by the presence of hip pain and a detailed examination. The incidence of iliacus hematoma may increase because of the widespread use of anticoagulant therapy and revision hip surgery. In otherwise healthy patients with incomplete femoral neuropathy secondary to traumatic iliacus hematoma, conservative treatment can achieve excellent results.
Reference: Kuo HW, Ku JW, Chiang CJ, Rau G, Chen CY, Chen CH. Complete femoral nerve palsy following traumatic iliacus hematoma: a case report and literature review. JBJS Case Connector. 2013 Jul 24;3(3):e74.
Aneurysmal bone cyst
Ewing sarcoma
Sarcoma involving the iliacus muscle
Iliacus hematoma
Pelvic abscess


 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3