A Patient with an Abdominal Mass After Metal-on-Metal Hip Replacement
September 18, 2013
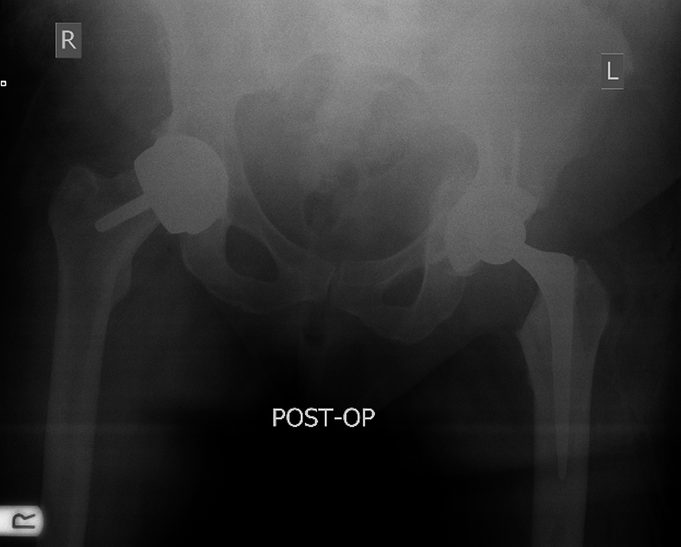
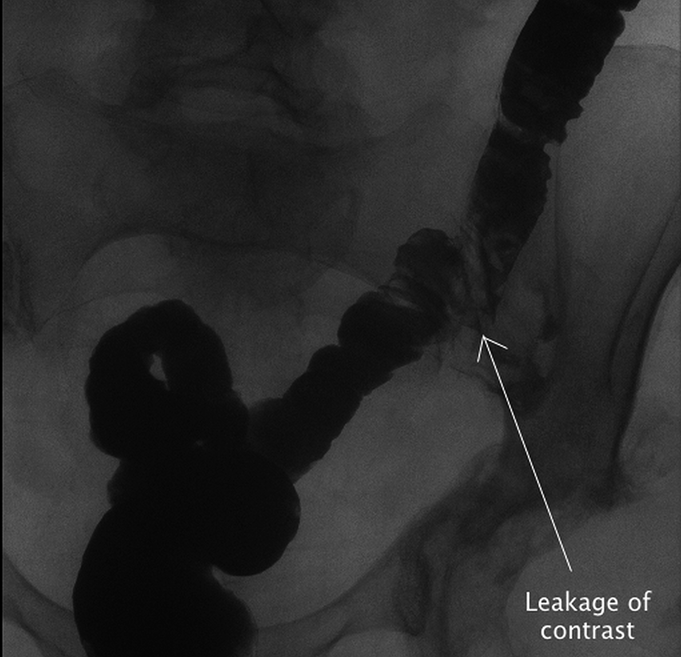
A fifty-nine-year-old woman with a six-week history of pain in the left lower quadrant of the abdomen that radiated to the left groin and thigh presented to our institution. She had no change in bowel habit and no history of febrile illness. The left hip had been painful for about six months. She had undergone a total abdominal hysterectomy and bilateral salpingo-oophorectomy and omentectomy for a left ovarian tumor eighteen months earlier. The histopathology report had revealed a borderline mucinous tumor confined to the left ovary. The history also included right and left Birmingham hip resurfacing (Smith & Nephew, Warwick, United Kingdom) arthroplasty for osteoarthritis, performed nine and five years earlier, respectively. These resurfacing arthroplasties, which were performed at a different institution, had no intraoperative or postoperative complications. On examination, there was a nontender mass in the left iliac fossa. Left hip movement was considerably restricted by pain. A radiograph of the pelvis showed bilateral Birmingham hip resurfacing without evidence of loosening (Fig. 1). A computed tomography (CT) scan of the thorax, abdomen, and pelvis was obtained. This showed a 6 × 7-cm complex heterogeneous mass involving the mid and distal portion of the left psoas muscle (Fig. 2). The left external iliac vein and artery were displaced by this lesion but did not appear to be involved. There were several enlarged internal iliac lymph nodes. The psoas mass had not been visible on CT or intraoperatively at the time of the total abdominal hysterectomy eighteen months earlier. Ultrasound-guided core biopsies were obtained, and the histology revealed abundant granular extracellular material of uncertain origin, amorphous eosinophilic material, fibrin, and degenerate muscle, although it was not diagnostic. Microscopy and cultures were negative for organisms. An exploratory laparotomy was performed by general surgeons via an abdominal approach. This revealed a large firm retroperitoneal tumor involving the left psoas muscle; the tumor was fixed to the iliac crest. The lesion extended along the psoas muscle under the ilioinguinal ligament and beyond the pelvis. It did not extend as far as the sciatic notch. No connection with the bowel was observed, and no iatrogenic visceral injury was discerned intraoperatively. Although the CT scan had suggested that the left external iliac vessels were displaced by the mass, the surgeons found that there was some involvement of these major vessels in the inflammatory mass; thus, it was unresectable. Histology of the biopsies showed nonviable amorphous eosinophilic cellular material adjacent to striated muscle and inflamed connective tissue. Microscopy and cultures were negative for organisms, including mycobacteria and fungi. The findings raised the possibility that the lesion was a pseudotumor associated with the resurfacing arthroplasty. Consequently, serum cobalt and chromium levels were measured and were found to be elevated (24.9 and 19.6 parts per billion [ppb], respectively [normal: 2.65 and 2.34 ppb for cobalt and chromium, respectively]).
Three months later, the patient had symptoms of clicking and instability in the left hip. On examination, there was no erythema or swelling around the hip, but active and passive hip movement was substantially limited by pain. A left hip arthroscopy was performed. Visualization inside the hip joint was difficult because of extensive fibrotic tissue. Turbid fluid was aspirated; microscopy and cultures were negative for organisms. After careful deliberation with the patient, it was decided to revise the left hip arthroplasty. Intraoperatively, turbid fluid was found deep to the fascia. Rubbery fibrous tissue was found around the trochanters, short hip rotator muscles, and iliopsoas tendon. The intra-articular fibrosis extended proximally into the area of the psoas mass. Because findings were consistent with pseudotumor rather than infection, it was decided to perform a one-stage revision. Intraoperative analysis of frozen sections to identify infection was not available at our facility. The resurfacing components were well fixed but were removed without difficulty. Defects were found in the roof and medial wall of the acetabulum. These were filled with impaction bone allograft. No attempt was made to resect the proximal extension of the pseudotumor along the psoas muscle for fear of iatrogenic vascular injury. A Regenerex titanium shell (Biomet Orthopedics, Warsaw, Indiana) with a polyethylene liner was impacted into the acetabulum and secured with multiple screws. The femoral side was revised with use of a cemented Exeter stem (Stryker Orthopaedics, Mahwah, New Jersey) (Fig. 3). Histopathological analysis of the excised tissue showed fibrosis and chronic inflammation. Postoperatively (within three hours), the patient became febrile, tachycardic, and hypotensive. She was treated with intravenous vancomycin and required noradrenaline for three days for blood pressure support. Intraoperative swabs grew coliforms and coagulase-negative staphylococci. A CT scan showed no fluid collection, but she continued to have fevers and was returned to the operating room. The wound was opened and pus was found deep to the fascia, tracking down to the hip joint. Several washouts and negative pressure dressing applications were undertaken over the next five weeks. The cultures grew Enterobacter cloacae and Enterococcus species, which were sensitive to vancomycin and gentamicin. The patient was treated with intravenous vancomycin (15 mg/kg every twelve hours) and piperacillin-tazobactam (4.5 g every eight hours). The infection persisted despite repeated washouts and antibiotics, and the patient underwent a left resection arthroplasty five weeks after the revision surgery; all of the implants were removed. Intraoperative swabs had positive cultures for Enterococcus faecium. Serum chromium and cobalt levels had now normalized to values of 4.1 ppb and 2.9 ppb, respectively. CT scans, a colonoscopy, and a gastrografin enema failed to show a colonic fistula, but enteric organisms persisted in the discharge from the wound. Finally, a repeat gastrografin enema revealed spillage of contrast from the sigmoid colon into the left iliac fossa with contained lateral spread, likely into the potential space within the pseudotumor (Fig. 4). A laparoscopic defunctioning loop ileostomy was performed, and a stoma was formed in the right iliac fossa. Subsequently, no additional fecal discharge was noted, and the wound was allowed to granulate by secondary intention. At the twenty-four-month follow-up, a small amount of clear discharge from the enterocutaneous fistula persisted; it was managed with daily dressings. The patient was afebrile and systemically well and had not required antibiotics for many months. She was able to mobilize short distances with a cane without hip pain. The most recent CT scan showed that the pseudotumor had decreased in size to 3 × 2.4 cm. The proximal sigmoid colon was abutting the lesion with tiny pockets of air at this level, suggestive of a persistent fistulous connection. There was interval reduction in the inflammatory changes surrounding the left hip joint. The patient was averse to any additional surgical intervention. She was willing to tolerate the colocutaneous fistula that persisted despite the ileostomy.
Proceed to Discussion >>Reference: Bruce-Brand R, Kennedy T, Gul R. Coloarticular fistula associated with a pseudotumor after metal-on-metal hip resurfacing arthroplasty: a case report. JBJS Case Connector. 2013 Jul 10;3(3):e67.
This case indicates the diagnostic difficulties and high morbidity associated with a pseudotumor after metal-on-metal hip resurfacing arthroplasty. The patient’s history of an ovarian tumor rendered diagnosis of an arthroplasty-associated pseudotumor more difficult. She had been admitted by the general surgeons, and the possibility that the pelvic mass was associated with the resurfacing arthroplasty was only raised after the laparotomy and subsequent histology and microbiology results. There were multiple predisposing factors to the development of a fistula in this patient. The previous gynecologic surgery, the exploratory laparotomy, the necrotic pseudotumor, and the revision hip arthroplasty were all risk factors. We believe that communication between the bowel and the hip joint likely occurred at the time of the revision hip arthroplasty. At the earlier time of the exploratory laparotomy, no bowel communication or adhesions to the bowel were seen, and the cultures of the intraoperative biopsies were negative. Fluid aspirated from the left hip joint during a subsequent hip arthroscopy and prior to the revision arthroplasty also yielded negative microscopy and cultures for organisms. The patient became septic immediately following the revision arthroplasty, and intraoperative and subsequent cultures grew enteric organisms. Although no iatrogenic injury to the bowel was discerned during the surgery, it is hypothesized that removing the acetabular component from an acetabulum that had substantial medial and superior defects and was encased in inflammatory tissue may have created a tear in the adjacent adherent bowel. Confirming the source of the infection proved difficult: CT scans, a colonoscopy, and the first gastrografin enema all did not reveal the origin. The fistula failed to seal off after the defunctioning ileostomy. The presence of the pseudotumor and the previous life-threatening sepsis from bowel perforation, likely secondary to adhesions between the colon and the inflammatory mass, were factors that complicated additional management. The general surgeons deemed the pseudotumor inoperable because of involvement of the external iliac vessels. Given the multitude of surgical procedures the patient had undergone, it was understandable that she was reluctant for additional invasive procedures. This case report suggests that pseudotumors should be added to the documented predisposing conditions for the rare formation of a fistula between the bowel and an implant following hip arthroplasty.
Reference: Bruce-Brand R, Kennedy T, Gul R. Coloarticular fistula associated with a pseudotumor after metal-on-metal hip resurfacing arthroplasty: a case report. JBJS Case Connector. 2013 Jul 10;3(3):e67.
Iliacus hematoma
Pelvic abscess
Pseudotumor of metallic debris
Iliac sarcoma
Ovarian cancer mass


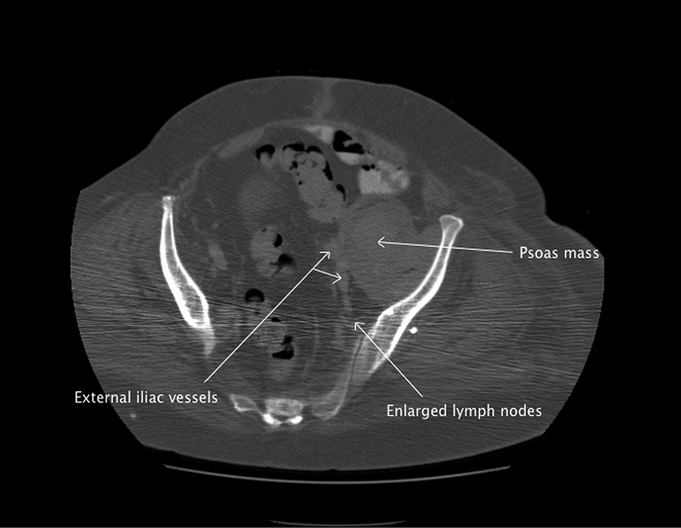
 Fig. 1
Fig. 1 Fig. 2
Fig. 2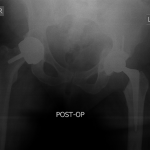 Fig. 3
Fig. 3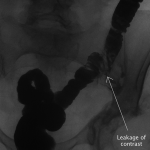 Fig. 4
Fig. 4