A Twenty-Year-Old Man with Right Lower-Extremity Pain
October 2, 2013
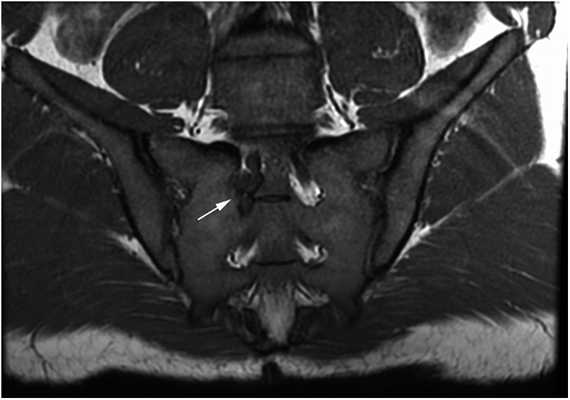
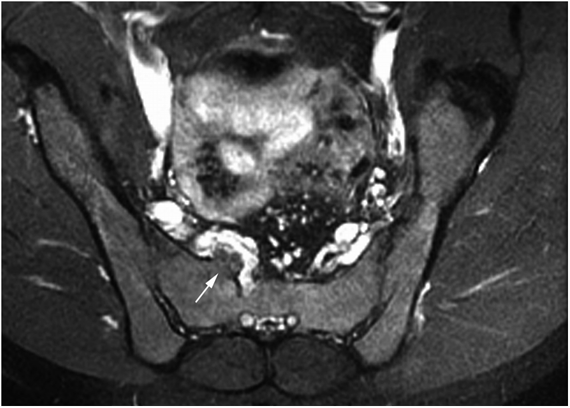
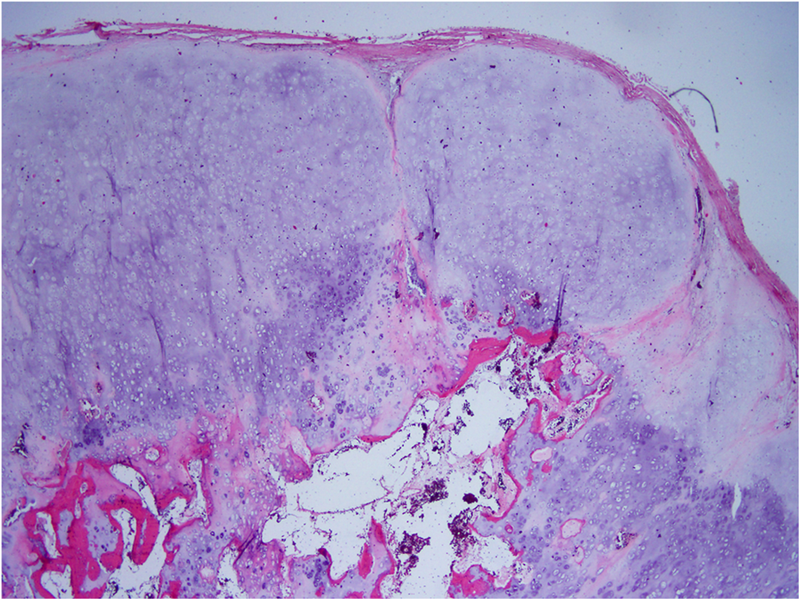
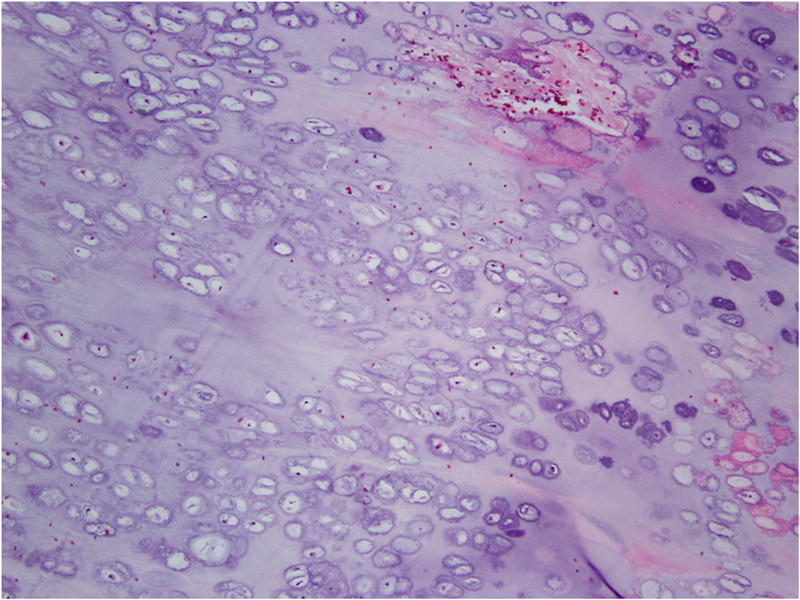
An otherwise healthy twenty-year-old male recreational soccer player presented with the symptom of six months of right leg pain. The history was noteworthy for prior back pain from a mild lumbar disc herniation on the right at the L4-L5 level, diagnosed with magnetic resonance imaging (MRI), which had been managed conservatively. For the six months prior to presentation, he reported experiencing a tingling and stabbing pain in the right buttock, posterior thigh, calf, and lateral aspect of the foot. He also had new onset of a “pins-and-needles” sensation in the lateral aspect of the right foot. The symptoms worsened with activity and prolonged sitting on hard surfaces. The patient stopped playing soccer secondary to severe stabbing leg pain. He denied muscle weakness, saddle anesthesia, bowel or bladder incontinence, weight loss, or night pain. Initial treatment was with physical therapy, nonsteroidal anti-inflammatory drugs (NSAIDS), and chiropractic manipulation, but, despite the conservative treatments, the symptoms continued to worsen over the next four months. Physical examination was notable for a healthy-appearing twenty-year-old man with normal painless range of motion in the lower extremities and normal bilateral lower-extremity strength. Examination of the lumbar spine demonstrated painless active forward flexion to 90° and extension to 30°, with side-to-side bending of 30°. Heel walking and toe walking were normal and symmetrical. He did report mild tenderness to palpation in the right sacroiliac region, distinct from the other pain symptoms. Pinprick examination demonstrated increased sensitivity in the S1 nerve root distribution. The deep tendon reflex of the right ankle was diminished. Pain was noted with the seated and supine straight-leg raise test and the Lasègue maneuver on the right side. The seated and supine straight-leg raise test on the left side did not evoke pain in either extremity. The patient denied pain with flexed abduction external rotation testing of the right leg. Radiographic imaging of the lumbosacral region and pelvis with plain radiographs did not clearly demonstrate a mass initially, although a vague abnormality in the region of the right proximal sacrum can be identified retrospectively. Computed tomography (CT) of the pelvis and lumbosacral junction was obtained (Figs. 1-A and 1-B).
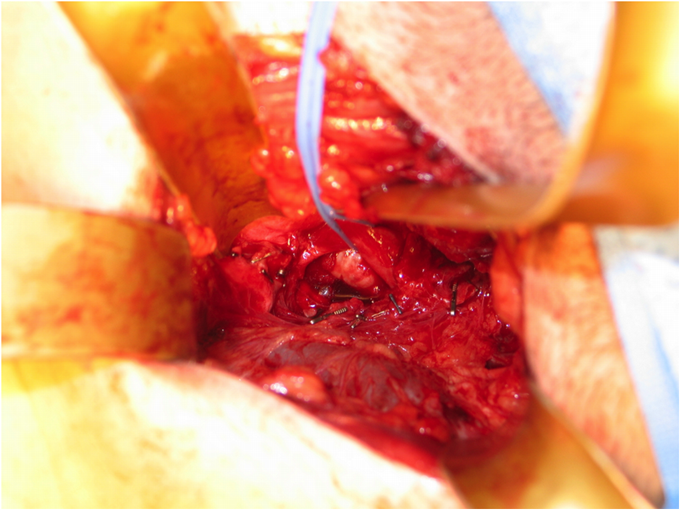
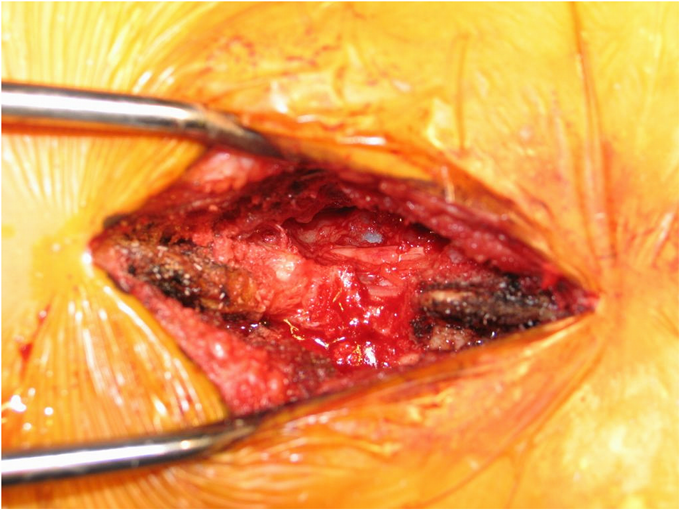
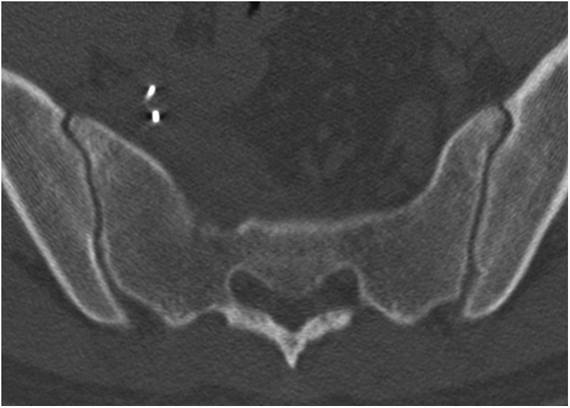
Prior to presentation to the surgical clinic, the symptoms had worsened despite the initial conservative management of physical therapy, NSAIDs, and chiropractic manipulation. For this reason, the patient was offered the option of excision, as a lesion and a mass were shown on preoperative MRI (Figs. 2, 3-A, and 3-B). Given the anterior, posterior, and foraminal extent of the tumor, a staged approach to excise the mass and decompress the nerve root was planned. First, the patient underwent surgical resection of the anterior exostosis lesion via a retroperitoneal approach to the sacrum through a modified Pfannenstiel incision. This portion of the procedure was performed by an orthopaedic oncologist and a general surgeon; it was chosen to be the first procedure primarily because of the availability of the combined surgical team. Exposure of the lesion demonstrated a well-defined osseous mass occluding the right S1 foramen (Fig. 4-A). The S1 nerve root appeared flattened and inflamed, and was overlying the tumor as the nerve exited the foramen. The anterior excision was performed with an osteotome; the base of the osteochondroma was cut, leaving only the intraforaminal and posterior portions of the mass. The second posterior stage of the procedure was performed by the orthopaedic oncologist and the spinal surgeon to remove the remainder of the mass and additionally decompress the S1 nerve root. Through a midline vertical incision and standard posterior sacrum and spinal exposure, the canal was entered and decompressed to the level of the ligamentum flavum with use of a high-speed burr and rongeur. The ligamentum flavum was removed. The nerve roots were retracted, and the posterior portions of the osteochondroma were removed with a rongeur. Cartilage was clearly visible in the canal when it was opened. The neural foramen was then enlarged with Kerrison rongeurs and curets. A Woodson probe was passed through the foramen and confirmed complete decompression of the stenosis caused by the lesion (Fig. 4-B). Histopathology confirmed the diagnosis of benign sacral osteochondroma (Figs. 5-A and 5-B). On postoperative day one following the posterior decompression, the patient reported substantial resolution of the lower-extremity pain on the right side, in particular the stabbing pain extending to the foot. In addition, he demonstrated intact sensation to light touch as well as 5/5 strength in all lower-extremity muscle groups. The postoperative CT showed that the cartilaginous cap had been removed and that there had been enlargement of the S1 neural foramen (Fig. 6). At the one-month follow-up, the patient reported complete resolution of the stabbing pain in the buttocks and the leg pain, with some persistent sensation of “pins and needles” in the foot; on examination, he had normal muscle strength and tone as well as normal sensation. At the two-year follow-up, the patient had no symptoms of leg pain, tingling, or loss of sensation, and he stated that he had been able to resume playing soccer. He did report mild occasional foot tingling, but not severe enough to warrant any medication. Neurologic examination of the bilateral lower extremities showed full strength and intact sensation to light touch in the distribution of the S1 nerve root, including the distribution of the gastrocnemius muscle, the soleus muscle, and the sole of the foot. Radiographs and MRI obtained at that time showed no recurrence of the osteochondroma.
Proceed to Discussion >>Reference: Maceroli M, Ponnappan R, Shallop B, Vaccaro A, Abraham J. Sacral foraminal osteochondroma causing radiculopathy: a case report. JBJS Case Connector. 2013 Jul 10;3(3):e70.
Primary sacral osteochondroma is a rare diagnosis in spinal surgery. To the best of our knowledge, less than ten cases have been cited in the literature. The authors used a retroperitoneal approach for excision of this lesion. All other reported cases illustrate posterior lesions causing lower back or sciatic nerve pain. In our patient, the lesion traversed the entire neural foramen with a cartilage cap extending from the spinal canal posteriorly through the foramen into the pelvis. On CT and MRI, an osteochondroma will characteristically display continuity with the medullary cavity of native bone, as seen in our patient. On MRI, the cartilaginous cap will demonstrate intermediate-signal intensity on T1-weighted images and high-signal intensity on T2-weighted images. Asymptomatic lesions can be observed. The only treatment option for symptomatic lesions is surgical excision, with the vast majority of patients reporting postoperative satisfaction. Only 1% to 5% of solitary osteochondromas undergo malignant transformation to secondary chondrosarcoma. Local recurrence following complete resection, continued growth despite skeletal maturity, and sudden increases in pain without evidence of neuropathy are concerning for malignant change. Current literature suggests that a cartilaginous cap thickness greater than 2 cm on T2-weighted MRI is worrisome for chondrosarcoma. In the literature, almost all patients with symptomatic sacral osteochondroma underwent tumor resection and dural sac decompression via a posterior approach. In the present case, the lesion’s bulk was anteriorly located on the sacrum, and resection was conducted through a modified Pfannenstiel incision. This allowed maximum exposure of the mass. We were able to remove the bulk of the mass through the anterior excision, but we were unable to sufficiently decompress the foraminal stenosis from the residual mass, necessitating the additional posterior exposure. We performed a posterior decompressive laminectomy and further excision of compressive posterior tumor remnants in the neural foramen to complete the excision. The second stage provided a means of removing the entirety of the remaining mass while protecting local neurovascular structures.
Reference: Maceroli M, Ponnappan R, Shallop B, Vaccaro A, Abraham J. Sacral foraminal osteochondroma causing radiculopathy: a case report. JBJS Case Connector. 2013 Jul 10;3(3):e70.
L5-S1 disc herniation
Sacral chordoma
L4-L5 disc herniation
S1 schwannoma
Osteochondroma of the S1 foramen

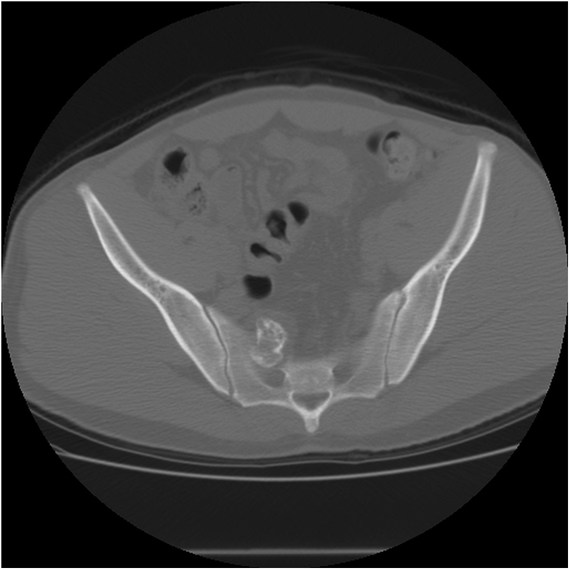
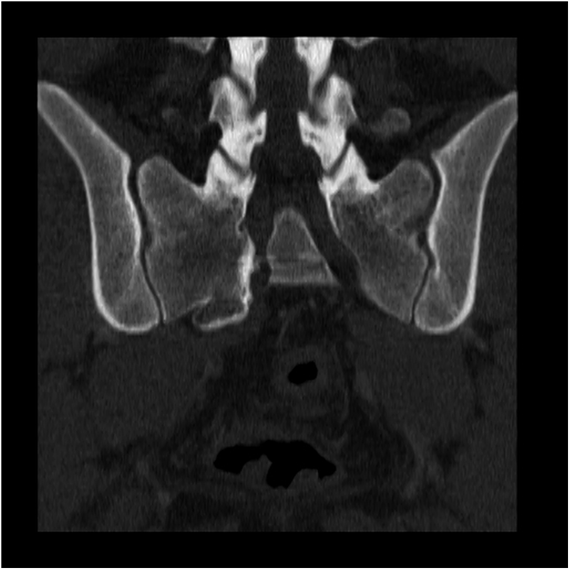
 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2
Fig. 2 Fig. 3-A
Fig. 3-A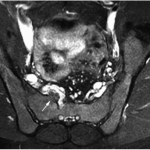 Fig. 3-B
Fig. 3-B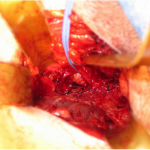 Fig. 4-A
Fig. 4-A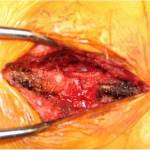 Fig. 4-B
Fig. 4-B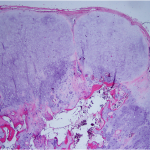 Fig. 5-A
Fig. 5-A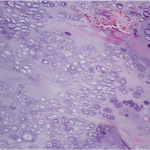 Fig. 5-B
Fig. 5-B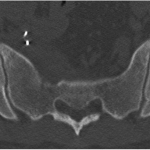 Fig. 6
Fig. 6