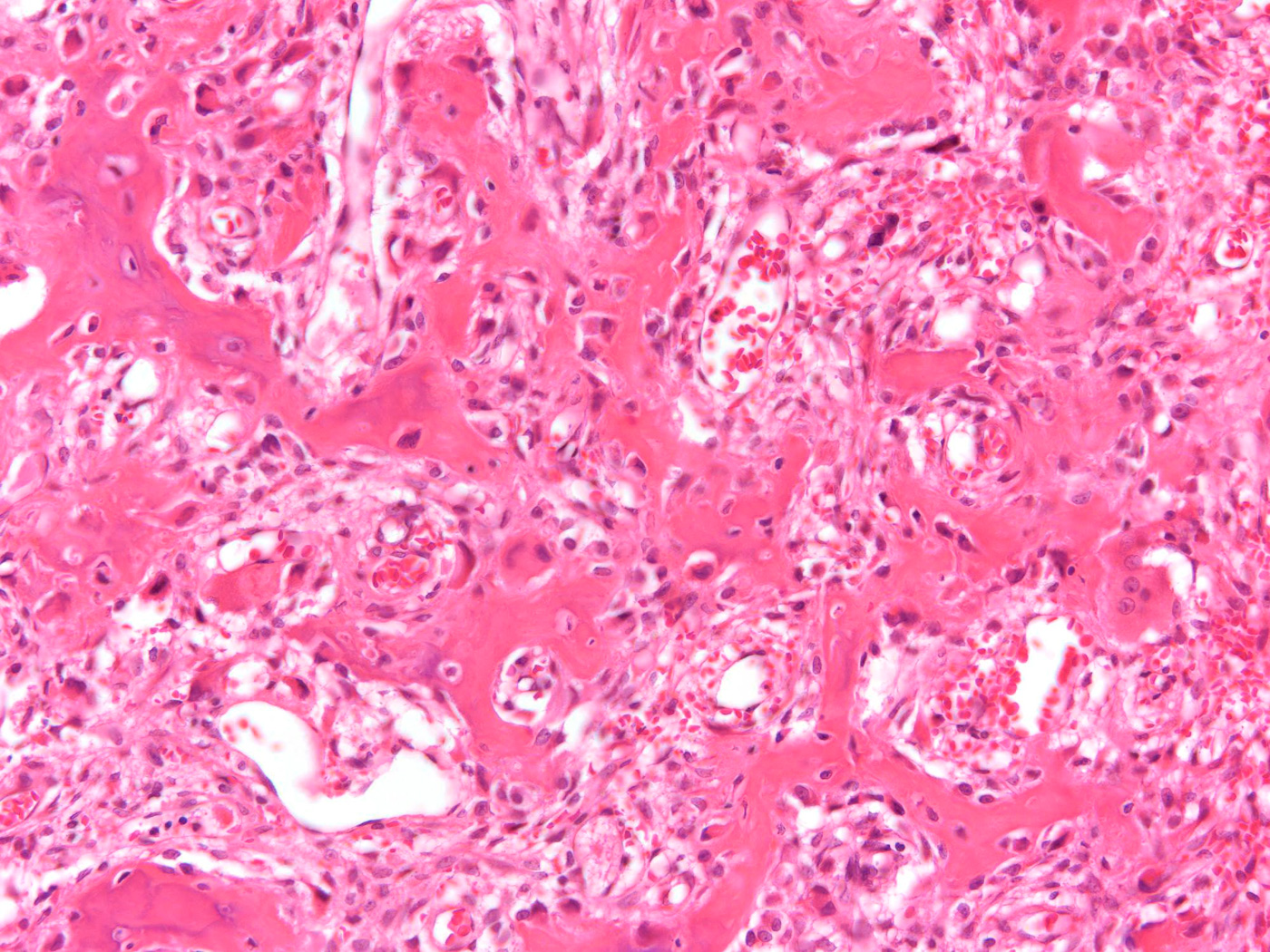
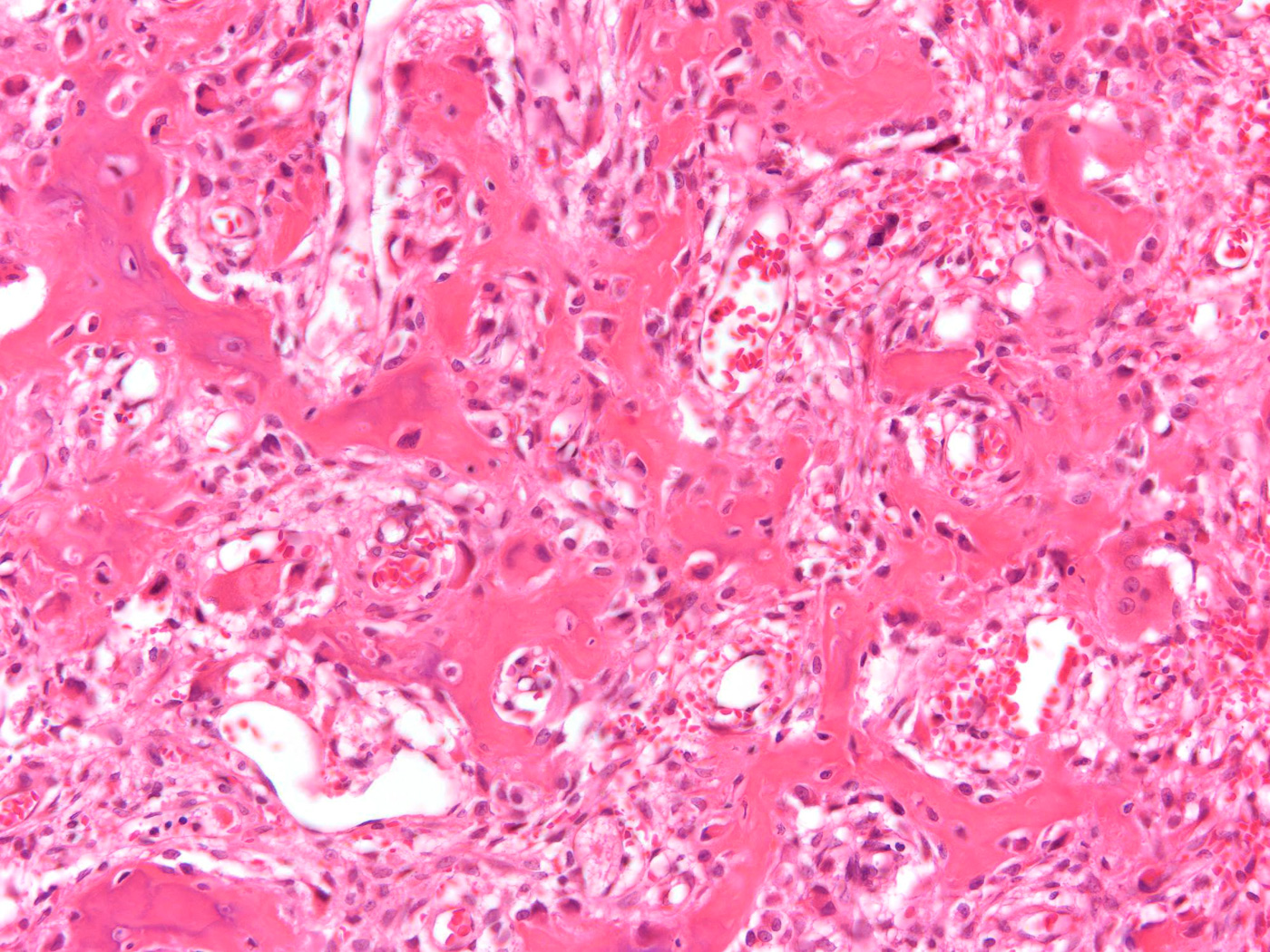
An otherwise healthy seven-year-old boy presented with a left tibial mass that was painful at night. The patient had a history of a fibrous hamartoma in the proximal part of the right arm in infancy; the lesion was removed at the age of two years without complication. A radiograph of the left lower limb demonstrated focal sclerosis in the proximal part of the tibial shaft (Fig. 1). A bone scan revealed an abnormality of the anterior medial aspect of the left proximal tibial metadiaphysis of uncertain etiology. No other areas of increased uptake were present. A computed tomography (CT) scan revealed an elongated lesion within the cortical thickening that measured 3 mm in greatest transverse dimension but approximately 2 cm in length (Fig. 2). The majority of the lucency was covered by a thick rim of cortical bone. With the patient under general anesthesia, a tissue core needle biopsy was performed under CT guidance. Pathological analysis confirmed the diagnosis of osteoid osteoma (Fig. 3). CT radiofrequency ablation was then performed through the same tract with a 5-mm radiofrequency probe that was heated to 90°C for six minutes. The patient tolerated the procedure well, and the pain decreased dramatically. The patient remained asymptomatic until he returned nine years later with a nine-month history of middle back pain of insidious onset. The pain was constant but not progressive. The patient reported night sweats as well as tingling of the feet. He also reported that the pain awakened him at night and was associated with difficult breathing. Magnetic resonance imaging (MRI) of the thoracic spine with and without gadolinium revealed reactive soft-tissue swelling to the left of the T6, T7, and T8 vertebral bodies, with a mildly increased T2 signal (Figs. 4-A and 4-B). The adjacent vertebral body of T7 had a mildly increased T2 signal and abnormal enhancement. No intraspinal extension or vertebral body destruction was found. Further evaluation with CT revealed a 1-cm rounded lesion in the left anterior part of the T7 vertebral body associated with adjacent sclerosis and soft-tissue swelling. There was minimal sclerosis of the adjacent anterior-superior part of the T8 vertebral body (Figs. 5-A and 5-B). A bone scan revealed focal high uptake in the left T7 vertebral body. A needle biopsy of the lesion was done (Fig. 6).
The diagnosis of osteoid osteoma was confirmed (Fig. 6) and a thoracic spine radiofrequency ablation was performed immediately thereafter (Fig. 7). At the time of the most recent follow-up, seven months after treatment, the patient remained symptom-free.
Proceed to Discussion >>Reference: Beck SE, Schwab JH, Rosenthal DI, Rosenberg AE, Grottkau BE. Metachronous osteoid osteoma of the tibia and the T7 vertebral body. A case report. J Bone Joint Surg Am. 2011;93:e73(1-5).
Multiplicity of osteoid osteoma is rare and may be explained in several different ways. The majority of cases take the form of "multiple niduses" in which multiple foci of tumor are found in a localized area, often entirely within the reactive zone of bone that is elicited by and surrounds the tumor. We believe that in some instances the appearance of multiple niduses results from partitioning of an elongated lesion into multiple, apparently discrete foci. This can explain the appearance of localized, multifocal osteoid osteoma. However, very rare instances of multiple synchronous tumors have been reported in adjacent bones and one case was recently reported to have occurred in remote bones. In the case of our patient, the tumors were anatomically distant and were separated in time by a nine-year interval. It is possible that this occurrence represents nothing more than a statistical coincidence. However, the location of the second lesion in the vertebral body is unusual. Although spinal osteoid osteomas are not rare, they are typically found in the posterior elements. We are aware of only a few instances of osteoid osteoma arising in the vertebral body. The atypical location raises the possibility that this patient may have a predisposition to form these tumors. It is conceivable that both lesions were present at the time of the initial presentation, with the spinal lesion being asymptomatic and therefore not detected. Despite the negative bone scan in the case of our patient, a small number of asymptomatic osteoid osteomas have been reported, which tend to be atypical in terms of location and patient demographics, raising questions about accurate diagnosis. In our patient, a healthy teenage boy, the lesion was certainly in an unusual location, but we believe that the histological diagnosis is secure. We find it improbable that a lesion would be present for nine years before the development of symptoms. Recurrence of osteoid osteoma after surgery has been reported in up to 11% of patients. In most instances, the recurrence is adjacent to the site of the initial tumor and is assumed to be due to incomplete removal of the lesion. Local recurrence after complete excision with clear margins, however, has also been documented. In the case of our patient, distant recurrence would have to be classified as metastasis, and the metastasis of an osteoid osteoma after a nine-year period is extremely unlikely. Both lesions in our patient were treated with radiofrequency ablation, a method that has been used for osteoid osteoma for approximately twenty years and is now widely accepted. Some cases of osteoid osteoma resolve spontaneously, and therefore some authorities have advocated a trial of expectant medical therapy with nonsteroidal anti-inflammatory drugs. However, the time required for resolution and the likelihood of resolution are unpredictable, and the availability of minimally invasive therapy with radiofrequency ablation makes prolonged medical treatment unattractive. The spinal lesion in particular demonstrates the advantage of this method, as an open surgical approach to the lesion would have had substantial morbidity for the patient. To our knowledge, Buluç et al. reported the only case of multicentric synchronous anatomically separated osteoid osteomas. A three-phase bone scan showed lesions in the wrist, the proximal part of the femur, and the superolateral aspect of the left orbit. The wrist lesion was confirmed histopathologically as an osteoid osteoma at the time of surgery, but because the patient was otherwise asymptomatic, the other lesions were diagnosed with CT and were not biopsied. A review of the literature revealed a total of ten reported cases of multiple osteoid osteomas that were all located in the same bone or adjacent bones. Two cases of multicentric synchronous osteoblastomas have been reported. We believe that the case of our patient represents the first report of multicentric metachronous osteoid osteoma.
Reference: Beck SE, Schwab JH, Rosenthal DI, Rosenberg AE, Grottkau BE. Metachronous osteoid osteoma of the tibia and the T7 vertebral body. A case report. J Bone Joint Surg Am. 2011;93:e73(1-5).
Tuberculosis
Osteoblastoma
Osteoid osteoma
Chronic recurrent multifocal osteomyelitis






 1
1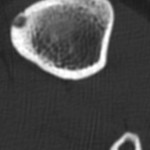 2
2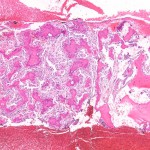 3
3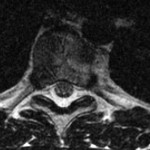 4-A
4-A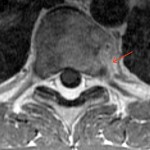 4-B
4-B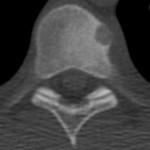 5-A
5-A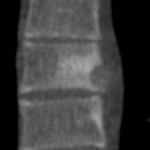 5-B
5-B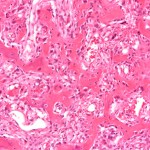 6
6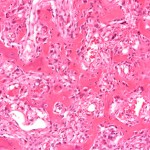 6
6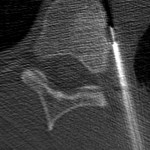 7
7