A Seventy-five-Year-Old Man with Left Leg Swelling and Hip Pain
September 21, 2011
A seventy-five-year-old man without major medical comorbidities was referred to our institution in April 2009 for evaluation and treatment of persistent edema in the left lower extremity in the setting of extrinsic femoral vein compression. The patient had undergone an uncomplicated primary metal-on-metal total hip arthroplasty for end-stage osteoarthritis at an outside hospital in November 2007. The arthroplasty was done with a 56-mm Durom acetabular cup, a 50-mm Metasul LDH femoral head, and a proximally coated M/L Taper stem (all components manufactured by Zimmer, Warsaw, Indiana). The postoperative recovery was uneventful, and the patient had been without symptoms until he presented to his primary-care provider twelve months later with the subacute onset of swelling in the left lower extremity and pain in the anterior aspect of the thigh. He had no history of metal hypersensitivity. Subsequent investigations included plain radiographs, which showed unremarkable findings, and a Doppler ultrasound examination, which showed no evidence of deep venous thrombosis but did reveal extraluminal compression of the femoral vein by a thigh mass. Computed tomography imaging demonstrated a periarticular fluid collection that had the appearance of a seroma or abscess. Aspirated fluid was negative for bacterial growth. A labeled autologous white-blood-cell scan revealed negative findings. In January 2009, the patient sought a second opinion in light of progressive swelling and worsening pain. Magnetic resonance imaging revealed fascial edema and signal abnormality in the medial and posterior compartments of the thigh surrounding the prosthesis. Fine-needle aspiration and core biopsies of the lesion revealed necrotic, dense fibrotic tissue with scattered fragments of metallic material. There was no evidence of malignant tumor, acute or chronic inflammation, or birefringence with polarization. In April 2009, on presentation to our institution for another opinion, the patient was afebrile without constitutional symptoms suggestive of an infectious process, although he had general malaise and a decreased appetite and had lost nearly 14 kg over the preceding five months. Physical examination revealed moderate, diffuse edema throughout the entire left lower extremity and a mass-like fullness in the posteromedial aspect of the thigh, adjacent to the groin. Plain radiographs demonstrated no evidence of implant loosening, although the acetabular component was not optimally positioned (Fig. 1). Acetabular cup inclination measured approximately 58°; the component was inferiorly placed and not medialized to the acetabular teardrop. Doppler ultrasonography showed a 6-cm mass adjacent to the hip joint compressing the common femoral vein. Gram staining of specimens obtained with guided aspiration of the hip joint was negative for organisms, and there was no bacterial growth on culture. Core needle biopsies of the soft-tissue mass showed no evidence of acute inflammation or malignant tumor. A magnetic resonance imaging scan (Fig. 2) showed diffuse thickening of the left hip joint capsule. The patient was scheduled for open biopsy and exploration of the mass. Approximately one week prior to his scheduled surgery, the patient presented to his local physician with foul-smelling yellow drainage from two new areas of soft-tissue breakdown overlying the left hip. He was empirically started on oral Augmentin (amoxicillin and clavulanate). During the operation, through a standard posterior exposure, marked diffuse thickening of the left hip joint capsule was seen with necrosis of the soft tissues extending from the subcutaneous fat directly down to the implant itself. Metallosis was not apparent. The femoral and acetabular components were loose and were easily removed; there was no evidence of osseous growth into either component. An articulating spacer consisting of antibiotic-impregnated cement was implanted. The biopsy of this mass is shown in Figure 3. Beta-hemolytic streptococci grew on microbiologic culture.
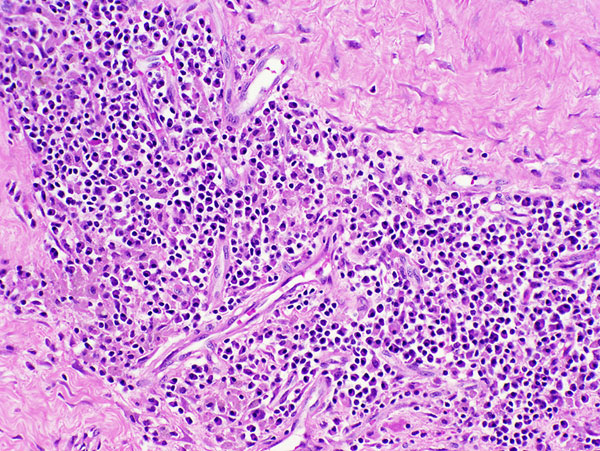
Histopathologic examination of intraoperative tissue specimens revealed metallic particulate matter with diffuse perivascular lymphocytic invasion, numerous plasma cells, and multifocal acute inflammation with extensive fibrinous necrosis. These findings demonstrated what appeared to be an acute inflammatory synovitis superimposed on a more chronic inflammatory process consistent with metal hypersensitivity, or ALVAL (Fig. 3). After an uncomplicated immediate postoperative course, the patient was discharged home, where he completed a six-week course of intravenous penicillin G. At his most recent evaluation, the patient was doing well and was without symptoms. The surgical wounds had healed without evidence of persistent infection, and the left lower-extremity edema and groin pain had largely resolved. The constitutional symptoms had resolved since removal of the metal-on-metal implant, and he had regained weight. He was offered implantation of a metal-on-polyethylene total hip replacement in place of his antibiotic-impregnated spacer.
Proceed to Discussion >>Reference: Watters TS, Eward WC, Hallows RK, Dodd LG, Wellman SS, Bolognesi MP. Pseudotumor with superimposed periprosthetic infection following metal-on-metal total hip arthroplasty. A case report. J Bone Joint Surg Am. 2010;92:1666-9.
Our patient underwent a metal-on-metal total hip arthroplasty and later presented with massive lower-extremity edema and groin pain secondary to compression of the femoral vein by an inflammatory pseudotumor. The underlying tissue reaction, with prominent perivascular lymphocytic infiltration, was consistent with ALVAL. A superimposed deep periprosthetic infection developed and represents a baleful consequence of delayed diagnosis. Metal hypersensitivity is an uncommon complication of metal-on-metal total hip arthroplasty and resurfacing arthroplasty, but it is an increasing cause of concern given the growing use of modern cobalt-chromium-molybdenum-alloy bearing surfaces for these procedures. In vivo, metal implant degradation leads to the release of metal ions that form immune complexes with native proteins, which can elicit local Type-IV hypersensitivity responses. Studies have demonstrated that corrosion at modular head-neck junctions could be a major source of metal debris, and it has been shown that increased cup inclination (for example, >50° in the frontal plane) can result in high serum levels of cobalt and chromium, presumably from excessive surface wear at the interface. In the present case, no obvious corrosion was present at the head-neck junction. From a technical standpoint, the acetabular cup inclination was excessive, measuring approximately 58°, and the cup was inferiorly placed and not well medialized. Inaccurate cup placement may have resulted in excessive metal-ion release due to wear, although notable metallosis was not readily apparent on exploration of the hip. However, Willert et al. did not establish a connection between the level of the immunologic tissue response and the amount of metal debris present in the local tissues. At revision, both the femoral stem and the acetabular cup were found to be loose and did not show evidence of osseous ingrowth on gross examination. Although there have been some reported cases of metal hypersensitivity with only soft-tissue involvement and unaffected bone-implant integration, aseptic loosening is a common manifestation of this disease process. There is no way to ascertain which came first in our patient—the ALVAL or the loosening. Multiple prior aspirations, biopsies, and a negative labeled white-blood-cell scan of the left hip suggest that a chronic infection was not the underlying cause of the loosening. While it is possible that the infection resulted from contamination of the joint during diagnostic tissue sampling, one would suspect that, if that had been the case, the infection would have developed in closer proximity to the sites of those procedures and with an organism that is more common to skin flora. Another unique feature of our case was the constellation of constitutional symptoms that resolved following removal of the prosthesis. To our knowledge, the generalized malaise, loss of appetite, and substantial weight loss experienced by our patient have not been reported previously, although Mikhael et al. described metal hypersensitivity mimicking infection in a patient who presented with low-grade fever, leukocytosis, and elevated levels of inflammatory markers. It is surprising that descriptions of such systemic symptoms in association with atypical periprosthetic hypersensitivity reactions are uncommon, since most other conditions associated with perivascular lymphocytic infiltration (for example, Takayasu arteritis and polyarteritis nodosa) are strongly associated with constitutional symptoms. This dichotomy underscores the observation by Willert et al. that it is not known if the perivascular infiltrates seen in ALVAL-type reactions represent a true vasculitis or a novel form of immunologic reaction. This lymphocytic reaction has been associated with surface tissue ulceration. It is possible that the sinus tracts and the ultimate breakdown of skin may have been the result of the underlying hypersensitivity reaction and the cause of the superimposed infection. Although the relationship between perivascular lymphocytic infiltrates and ulceration of adjacent tissue is poorly understood, Willert et al. noted that synovial fluid retrieved from hips with metal-on-metal implants is toxic to human fibroblasts in culture. This may explain the extensive tissue necrosis and ultimate skin breakdown seen in our patient. The vast majority of patients who undergo metal-on-metal arthroplasty appear to have no obvious reactions, and metal hypersensitivity reactions remain a rare phenomenon. Nevertheless, the variable presentation of these implant failures requires orthopaedic surgeons to be wary of the complication when a patient with metal-on-metal implants presents with unexplained pain following surgery. Although this case report portrays an association among a metal-on-metal articulation, pseudotumor, component loosening, and infection following diagnostic sampling, causality cannot be proven. Nevertheless, the delay in diagnosis and implant removal at the very least provided no benefit to this patient. We propose that patients with metal-on-metal bearing surfaces and potential periprosthetic pseudotumor undergo soft-tissue imaging and biopsy early in the course of diagnostic evaluation. When such tissue sampling is suggestive of an atypical metal hypersensitivity reaction, proceeding directly to component revision may be preferable to continued observation.
Reference: Watters TS, Eward WC, Hallows RK, Dodd LG, Wellman SS, Bolognesi MP. Pseudotumor with superimposed periprosthetic infection following metal-on-metal total hip arthroplasty. A case report. J Bone Joint Surg Am. 2010;92:1666-9.
Low-grade infection from skin contaminant at the time of initial arthroplasty
Pseudotumor formation likely caused by excessive acetabular cup inclination
Metal hypersensitivity due to excessive femoral component varus
Granulomatous reaction to bone debris from the time of initial arthroplasty

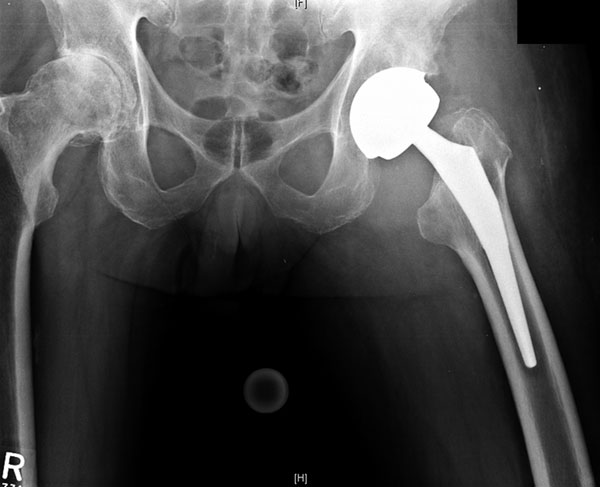
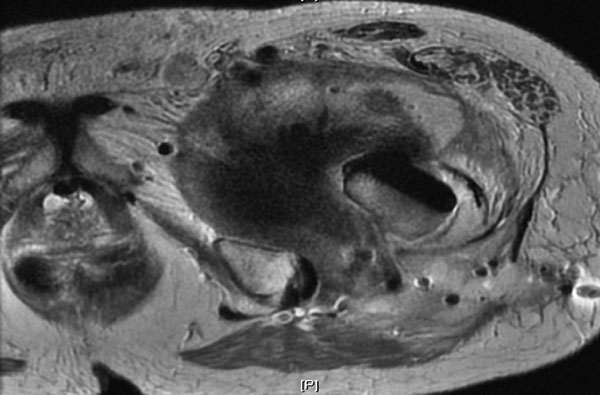

 Fig. 1
Fig. 1 Fig. 2
Fig. 2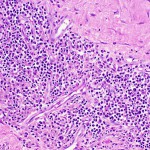 Fig. 3
Fig. 3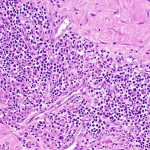 Fig. 3
Fig. 3