A Twelve-Year-Old Boy with Mid-Back Joint and Leg Weakness
October 5, 2011
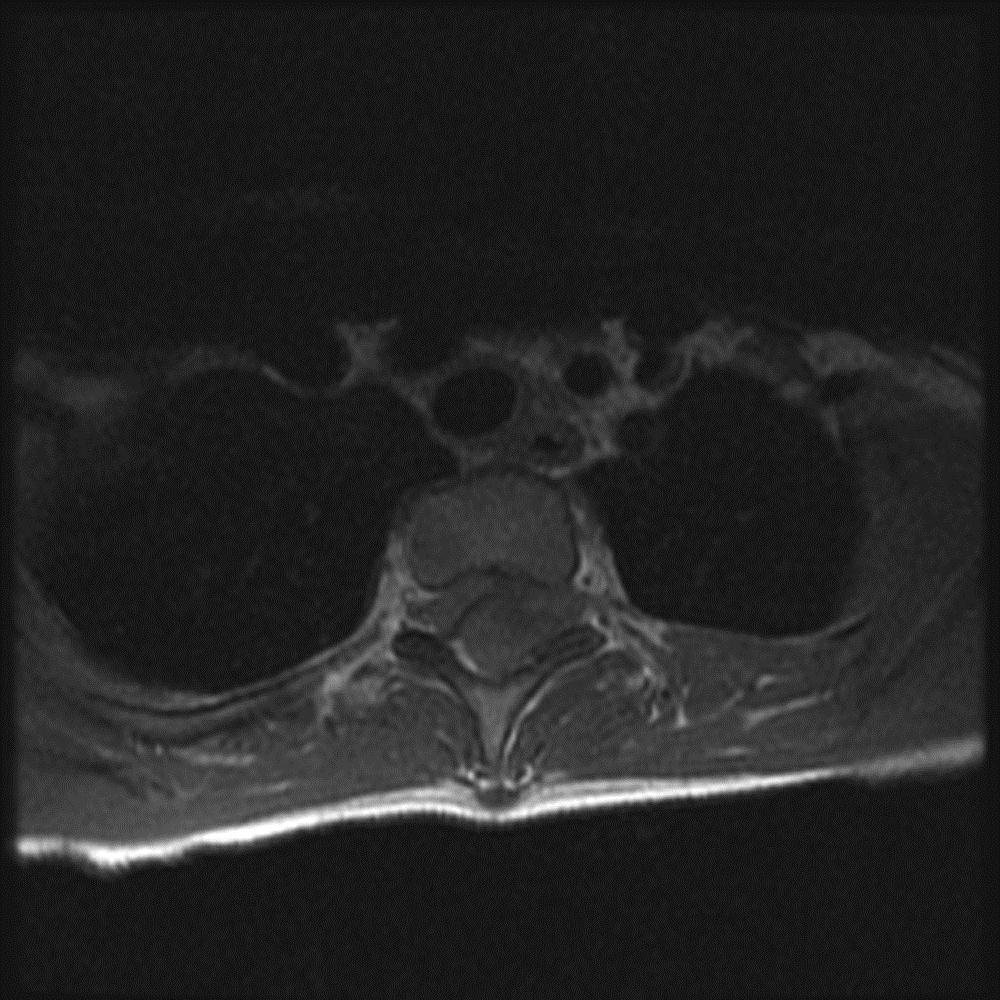
A twelve-year-old previously healthy boy presented to a hospital with complaints of intense back pain as well as bilateral numbness and tingling in the lower extremities. The only antecedent trauma had occurred three weeks prior to presentation. The patient was found to have a loss of motor function in both legs and was transferred to the emergency department of our hospital. On examination, he had no motor function in either lower extremity, had a loss of sensation caudad to the nipple line, and had priapism. On questioning, his parents stated that the boy had been pushed face first into a wall by another student at school; he was able to brace himself with his hands, and the impact was minimal. There was no apparent injury at that time. The patient began to have thoracic back pain and spasms five days later and saw his primary-care physician, who noted chest and shoulder pain but no neurological deficit. The patient was sent home with instructions for symptomatic treatment. Sixteen days after the incident, the patient once again presented to a health-care provider because of continued chest pain and symptoms of an upper respiratory illness, but no neurological deficit was noted. At the time of that visit, a radiograph of the chest showed no appreciable abnormality. Twenty-one days after the initial incident, the patient presented to another hospital, stating that he had had acute worsening of the back pain at school earlier that day and that, by the time he returned home from school, he had begun to feel numbness and tingling in his feet. He was urgently taken to the emergency department, where it was noted that he had flaccid paralysis involving the lower extremities bilaterally as well as decreased sensation caudad to the nipple line. The patient was then transferred to our emergency facility. Emergency magnetic resonance imaging was done (Figs. 1-A through 1-D).
Magnetic resonance images acquired at our facility revealed a large, dorsally located, epidural hematoma extending from the junction between C7 and T1 to the lower T4 vertebral body as well as considerable spinal cord compression. Edema of the spinal cord was seen at the T2 and T3 levels (Figs. 1-A through 1-D). The patient was taken to the emergency operating room, where he underwent a bilateral laminectomy of T1, T2, and T3 and evacuation of the hematoma. Complete decompression was completed approximately eight to nine hours after the onset of paralysis. Intraoperatively, the hematoma had both an organized clot as well as active bleeding, but no arteriovenous abnormalities were noted. The active bleeding was treated with bipolar cautery and by the application of thrombin-soaked gel foam and cottonoid patties. A minor amount of bleeding continued after treatment, and a drain was placed deep to the fascia on wound closure. Histologic analysis revealed hematoma. Further workup for a diathesis to bleeding revealed no abnormality. At the time of discharge from the hospital as well as eight months after operative intervention, the patient continued to have no improvement in the neurological level of paralysis despite aggressive rehabilitation.
Proceed to Discussion >>Reference: Lehman AAR, McKenna ME, Wisneski R, Hess WF. Delayed presentation of a traumatic spinal epidural hematoma in a preadolescent. A case report. J Bone Joint Surg Am. 2011;93:e28(1-4).
Back pain in the adult population tends to be predominantly degenerative in nature, whereas back pain in the pediatric population may be due to developmental disorders, infectious or inflammatory causes, or neoplastic disease. Injuries to the thoracic and lumbar spine, especially epidural hematomas, are relatively uncommon in children. Traumatic spinal epidural hematoma was first reported in 1827 by Morgan and Tyrrell. Symptoms usually include an acute onset of back or radicular pain followed by a progressive motor paralysis and sensory loss in the lower extremities. Progression from the onset of symptoms to neurological deterioration can take minutes, hours, or days. It has been noted that pain may be present for weeks before neurological deterioration begins. The patient had a delayed presentation of three weeks after the likely inciting incident. Previous reports related to delayed presentations are limited and have involved spontaneous spinal epidural hematoma. The cause of spontaneous spinal epidural hematoma is thought to be related to the extensively thin-walled and valveless venous plexus of the epidural space, which is vulnerable to rupture with sudden changes in venous pressures. Changes in intrathoracic pressure have been postulated to increase the venous pressures and possibly cause the epidural hematoma, especially if there is preexisting weakness. Activities such as voiding, sneezing, bending, and coughing may cause such events. The patient complained of a cough and cold symptoms five days prior to presentation. Whether or not this could have exacerbated an underlying weakness due to the initial trauma is unclear, although a possibility. Arterial sources of bleeding have also been suggested. Diatheses to arteriovenous malformations and bleeding may be causes of spontaneous spinal epidural hematoma; however, the patient was found to have no evidence of malformation and no diathesis to bleeding was identified. Magnetic resonance imaging is recognized as the preferred imaging modality to localize and qualify spontaneous spinal epidural hematoma. On magnetic resonance imaging, a subacute hematoma will appear with increased signal intensity on all imaging sequences due to the accumulation of methemoglobin. If the hematoma is chronic in nature, the by-product of the hemoglobin breakdown, hemosiderin, will appear as having a low signal intensity on all imaging sequences. However, if there are multiple stages of hematoma present, as was the case with this patient, then heterogeneous signal intensity can be appreciated. There was a lack of osseous disruption in the patient. This is possible in the pediatric population because the spinal column in that age group possesses greater elasticity, thereby allowing minor trauma to cause localized tearing of the epidural venous plexus. The majority of spontaneous spinal epidural hematomas are located dorsal to the spinal cord and in the cervicothoracic region, as was the case with this patient. Ventral to the spinal cord there is minimal space due to the dural sac being tightly apposed against the osseous canal, whereas dorsally this space is filled with fatty tissue. Foo and Rossier noted that, with the lack of osseous disruption, damage surrounding the spinal cord appeared to occur more often and the interval between trauma and an onset of neurological symptoms was prolonged as compared with the interval for patients who had osseous disruption. With spinal cord edema, as with this patient, the prognosis was worse. Surgical decompression remains the mainstay of therapy for spontaneous spinal epidural hematoma. Authors have described certain indications for conservative treatment, such as stable condition of a patient who has minimal neurological dysfunction, evidence of resolution of the hematoma, and no appreciable spinal cord compression, although instances in which these indications are present may be rare. The contributing factors to the overall prognosis and recovery of the patient include the preoperative neurological deficit (incomplete versus complete) and the interval of time until operative intervention. There is no clear consensus in the literature on the optimal time until operative intervention. Multiple opinions have been expressed, and suggestions are often dependent on the severity of the presenting neurological deficits. In their analysis of twenty-three cases of spontaneous spinal epidural hematoma, Liu et al. found that, when a complete deficit was present, the majority of cases resulted in a disappointing prognosis, even when some patients had surgical treatment less than twenty-four hours from onset of the neurological deterioration. On the contrary, when the patient had incomplete deficits, delayed operative intervention could still result in improved prognosis, sometimes even when the intervention was delayed for several days. In their investigation of fourteen patients who underwent hematoma removal because of spontaneous spinal epidural hematoma, Shin et al. found that, when incomplete neurological deficits were present, overall good outcomes were obtained when operative intervention took place less than twenty-four hours after the onset of neurological deterioration and that particularly good outcomes to normal function could be restored when the intervention took place less than twelve hours after the onset of neurological deterioration. However, if the patient had a complete deficit, even intervention in less than twelve hours could not ensure full recovery. The patient’s operative decompression occurred approximately eight to nine hours after the onset of neurological deterioration. However, at the time of his presentation at our facility, he had a complete neurological deficit, involving a loss of motor function in the lower extremities bilaterally and a loss of sensation caudad to the T3-T4 dermatomal distribution. As of eight months after the operative intervention, the patient had no improvement in his neurological level of paralysis despite aggressive rehabilitation. Spinal epidural hematomas are a rare entity in the pediatric population but are associated with considerable morbidity if overlooked. A high index of suspicion is often needed, but unremitting pain, even minor in intensity, or subtle neurological deficits should increase the index of suspicion. Magnetic resonance imaging should be acquired as soon as possible when patients with back trauma, no matter how minor, begin to have paresis or sensory abnormalities, even if osseous disruption is absent. When spinal epidural hematoma is discovered early, operative decompression yields promising results, but timely intervention is necessary because prolonged delay may result in unrecoverable deficits.
Reference: Lehman AAR, McKenna ME, Wisneski R, Hess WF. Delayed presentation of a traumatic spinal epidural hematoma in a preadolescent. A case report. J Bone Joint Surg Am. 2011;93:e28(1-4).
Epidural hematoma
Ependymoma
Arteriovenous malformation
Astrocytoma




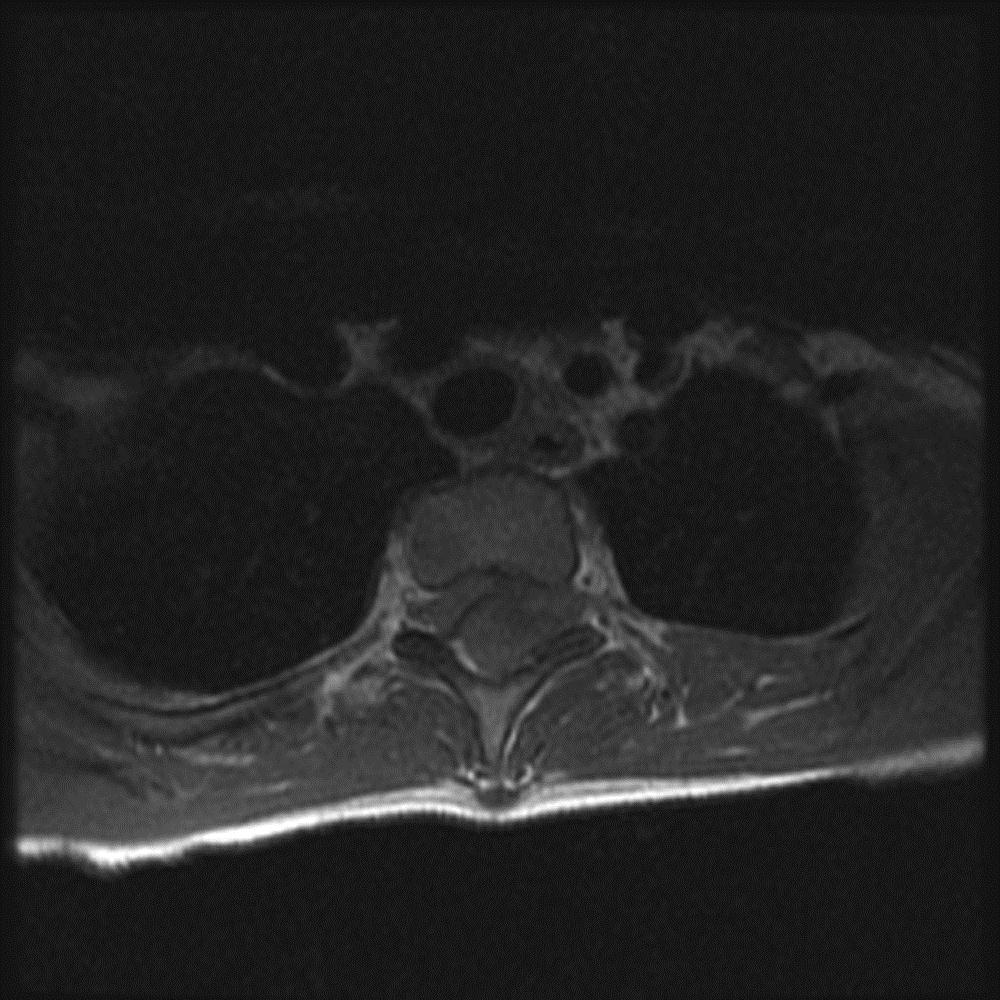
 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 1-C
Fig. 1-C Fig. 1-D
Fig. 1-D Fig. 1-A
Fig. 1-A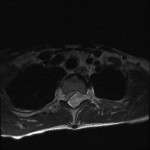 Fig. 1-B
Fig. 1-B Fig. 1-C
Fig. 1-C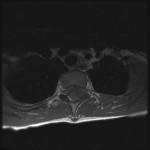 Fig. 1-D
Fig. 1-D