A Thirty-three-Year-Old Man with Wrist Pain for Three Months
May 4, 2011
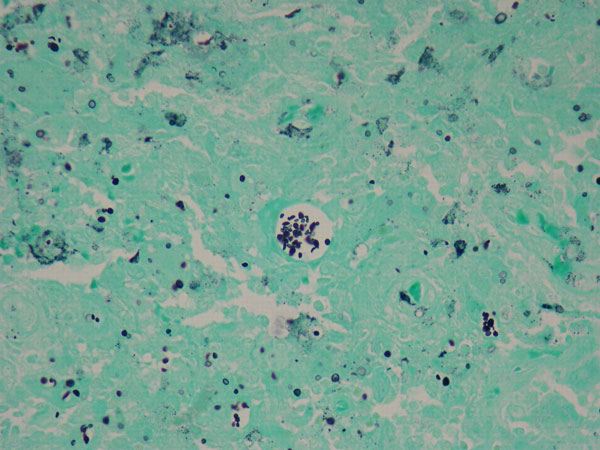
A thirty-three-year-old, right-hand-dominant, otherwise healthy man presented to the orthopaedic clinic with an approximately three-month history of pain in the left wrist. The patient denied any history of recent trauma to the extremity and reported no respiratory or systemic illness preceding the wrist pain. The medical history was notable only for an uneventful recovery following a gunshot wound to the left second metacarpal years earlier. He reported no fever, chills, or other constitutional symptoms and had recently screened negative for the human immunodeficiency virus (HIV). He had moved back to Memphis, Tennessee, six years before presentation after having lived in Dallas, Texas, for several years. Physical examination revealed that the patient was afebrile and that the vital signs were within normal limits. Examination of the left wrist revealed tenderness to palpation over the distal part of the radius but no palpable masses or overlying skin changes. The patient had full range of motion of the wrist. He was neurologically intact and had a palpable radial pulse. The white blood-cell count was 3600 µL (3.6 × 109/L), and the hematocrit was 39%. Radiographs of the wrist demonstrated a radiolucent lesion in the lateral aspect of the distal radial epiphysis, with sharp borders and mild cortical thinning (Figs. 1-A, 1-B, and 1-C). Open biopsy of the lesion was performed. Grossly, the lesion was composed of soft, reddish-brown tissue. The intraoperative frozen section revealed multinucleated giant cells with monotonous mononuclear stromal cells (Fig. 2-A). The lesion was removed with curettes. The cavity was then treated with a power burr, followed by an argon beam coagulator. The cavity was then filled with gentamicin-impregnated polymethylmethacrylate bone cement (Fig. 3). The wound was closed, a splint was applied, and the patient was discharged with outpatient follow-up.
On the fourth postoperative day, histologic examination demonstrated small budding yeast on Grocott-Gomori methenamine-silver nitrate and periodic acid-Schiff, digested stains, findings that were diagnostic of fungal osteomyelitis (Fig. 2-B). The morphological appearance was consistent with Histoplasma capsulatum, although fungal cultures were negative. A final mucicarmine stain was negative for additional fungal pathogens. The patient was readmitted to the hospital, and consultation with the infectious disease service was obtained. On further questioning, there were no identifiable risk factors for extrapulmonary histoplasmosis. The white blood-cell count ranged from 3900 µL (3.9 × 109/L) to 4900 µL (4.9 × 109/L), the erythrocyte sedimentation rate was 61 mm/hr, and the C-reactive protein level was 1.92 mg/dL (0.19 mg/L). Plasma coccidioidomycosis and urine blastomycosis antigen screens were negative. Urine antigen testing for systemic histoplasmosis, blood cultures, and repeat serological testing for the human immunodeficiency virus were also negative. Anteroposterior and lateral chest radiographs revealed a non-acute, mildly increased right lung interstitial pattern consistent with previous histoplasmosis exposure but not diagnostic for active disease. The patient initially was managed with intravenous amphotericin B with oral itraconazole but experienced acute renal insufficiency and fevers within twenty-four hours after the initiation of this regimen. The amphotericin B was therefore discontinued. The infectious disease service recommended oral itraconazole (200 mg, twice daily) for twelve months, and the patient was discharged on this regimen. The patient remained compliant with the oral antifungal regimen, and at the time of the twenty-three-month follow-up, he was doing well. He reported occasional mild pain in the distal part of the left radius but was otherwise able to perform the activities of daily living with very little difficulty. The wound was well healed, and the distal part of the radius was nontender. The patient had full pain-free range of flexion and extension of the wrist, with 70° of pronation and 80° of supination. Radiographs showed no signs of recurrence or fracture, and the cement remained in good position (Figs. 4-A and 4-B).
Proceed to Discussion >>Reference: McCabe MP, Heck RK. Histoplasma osteomyelitis simulating giant-cell tumor of the distal part of the radius. A case report. J Bone Joint Surg Am. 2010;92:708-14.
The case of our patient highlights the diagnostic dilemma often presented by musculoskeletal infections, particularly those caused by uncommon pathogens. This young, healthy patient was an unlikely host for such a rare infection, and the case described here underscores the importance and potential difficulties of accurate tissue diagnosis in cases of suspected neoplasia. Subacute osteomyelitis has long been known to present a diagnostic challenge because the medical history may lack findings that are indicative of infection and radiographs can suggest neoplastic processes. Bacterial pathogens, primarily Staphylococcus, remain the most common cause of subacute osteomyelitis in immunocompetent individuals, but mycotic infection does occur infrequently. Histoplasmosis is caused by Histoplasma capsulatum var. capsulatum, a dimorphic fungus endemic to the American Midwest and Southeast and classically associated with the Ohio and Mississippi River valleys. The fungus lives in soil contaminated with bird or bat excrement and can infect humans when its spores are aerosolized. North American histoplasmosis is a different condition than African histoplasmosis, the latter of which is endemic to Africa, is caused by Histoplasma capsulatum var. duboisii, and more commonly affects osseous and synovial structures. Recent phylogenetic research indicates that there may, in fact, be as many as eight subspecies of histoplasmosis globally and that the current nomenclature is outdated. Nevertheless, traditional distinctions based on the geographic and clinical characteristics of North American and African histoplasmosis remain accurate because these characteristics are reflections of fundamental genetic differences. Most histoplasmosis infections are pulmonary infections caused by the inhalation of spores and are asymptomatic or are associated with only mild symptoms. As many as 80% to 90% of residents in endemic areas have been infected; the prevalence of histoplasmosis in the United States is on the order of tens of millions. The severity of the primary infection depends on several factors, including the size of the inoculum, the immune status of the host, and the virulence of the infecting strain. Influenza-like symptoms such as fever, cough, and malaise are typical, although arthralgias are associated with primary infection during epidemics. Arthralgia is caused by the initial sensitization process during the inflammatory phase of the disease and resolves with nonoperative measures. Chronic, low-grade pulmonary histoplasmosis may result, occurring almost exclusively in patients with emphysema or other preexisting pulmonary disease. Systemic and disseminated histoplasmosis occurs as well, particularly in infants and immunocompromised hosts who have defects in cell-mediated immunity. An international consensus on endemic fungal infections defined pulmonary, systemic (extrapulmonary), and disseminated disease in cancer patients and stem-cell transplant recipients. Disseminated histoplasmosis is marked by pulmonary or systemic infection as evidenced by either positive blood cultures or positive serum or urine antigen testing. Extrapulmonary histoplasmosis is an AIDS (acquired immunodeficiency syndrome)-defining illness in HIV-positive individuals but still only rarely involves the musculoskeletal system. Septic arthritis of the knee has been reported in at least two AIDS patients. The diagnosis of histoplasmosis is made by identifying Histoplasma capsulatum yeast cells on histological analysis or by isolating the fungus on culture, and it can take weeks for the culture to become positive. Skin testing with histoplasmin antigen is not useful for diagnosis because previous infection is so common in endemic regions. Confirmatory testing with DNA-assay techniques or serological studies is indicated once a presumptive histological diagnosis of Histoplasma is made as the small (2 to 4-µm) narrow-based microconidia and larger (8 to 15-µm) macroconidia may be confused with other mycoses, including Candida glabrata, Leishmania, and Sepedonium. Sporothrix schenckii, which has similar-size (3 to 6-µm) cigar-shaped microconidia, presents with characteristic ulcerative lymphocutaneous lesions in at-risk patients, with isolated osteoarticular infection being very rare. Most published reports of musculoskeletal involvement have described patients with systemic or disseminated histoplasmosis. Bone-marrow infection has been identified frequently, a result of the diffuse involvement of the reticuloendothelial system in cases of disseminated disease, but osseous involvement is otherwise rare. Septic arthritis has been reported, with seeding of the joint presumably occurring by means of hematogenous spread after pulmonary infection. Three cases of fatal, disseminated histoplasmosis in infants, reported in the 1950s, provided the best radiographic details of osseous histoplasmosis. Long bones were noted to have cortical thickening, with pronounced periosteal reaction; flat bones demonstrated multiple osteolytic lesions. Histoplasma presenting as synovitis of the wrist, typically flexor tenosynovitis or carpal tunnel syndrome, appears to be the most common musculoskeletal manifestation of histoplasmosis in healthy patients. However, bone involvement was definitely identified in only two of eleven reported cases. Histoplasma capsulatum osteomyelitis without concomitant synovial or articular involvement has rarely been reported in the literature, with only three cases identified in our review. One of these patients had diagnosed pulmonary disease, and another had a history of non-Hodgkin lymphoma and chronic chemotherapy. The third patient was otherwise healthy but presented at the age of sixty-seven years. Thus, the case described here appears to represent the first reported case of isolated histoplasmosis osteomyelitis in a young, otherwise healthy patient. Unlike many patients described in the literature, our patient had no history of previous immunosuppression during which an indolent infection may have established itself. The presentation was also of interest because both the preoperative radiographs and the intraoperative frozen section suggested a diagnosis of giant-cell tumor of the distal part of the radius. The surgical treatment was individualized to this diagnosis and, therefore, was also unique. The case described here as well as our review of the literature suggests that local debridement in conjunction with long-term oral itraconazole is an effective treatment for isolated Histoplasma capsulatum osteomyelitis. Furthermore, a review of the literature on musculoskeletal histoplasmosis in general indicates that operative debridement, when possible, combined with systemic antifungal treatment, yields the lowest chance of recurrence. Because of the rarity of isolated musculoskeletal involvement, specific treatment guidelines are not made in the 2007 update of the Clinical Practice Guidelines for the Management of Patients with Histoplasmosis. However, reasonable conclusions can be drawn from the recommendations. Amphotericin B is indicated for the treatment of disseminated disease in ill patients; however, it has an extensive side-effect profile and requires inpatient intravenous administration with close monitoring of renal function. Oral itraconazole (200 mg once or twice daily for six to twelve months) is therefore the drug of choice for mild and isolated disease. It is commonly used for chronic suppressive therapy for AIDS patients and was reported to be effective for chronic suppression in the case of one ill patient with a histoplasmosis infection at the site of a prosthetic hip. In patients who cannot take itraconazole, fluconazole (400 to 800 mg daily) is an alternative. Finally, long-term follow-up is advisable as musculoskeletal histoplasmosis has been shown to recur after long periods of latency. The case of our patient also highlights the importance of a collaborative approach to treatment by the surgeon, pathologist, and infectious disease specialist. Although this case occurred in an endemic region, the consulting services remained attentive to the possibility of concomitant infection with other fungal pathogens more commonly associated with osteomyelitis. Although the treatment of these infections is beyond the scope of this review, therapy often requires amphotericin B. Thus, once other mycoses were ruled out, oral therapy alone was recommended in light of the patient's mild symptoms and poor tolerance of amphotericin B. In addition, consultation with the pathologist can provide greater confidence in the diagnosis. Our patient, who lived in an endemic region, had findings on a chest radiograph that were consistent with previous Histoplasma exposure and lacked historical or clinical findings suggestive of infection with other histologically similar pathogens such as Sporothrix or Leishmania. At the time of diagnosis, DNA-based diagnostic tests were not readily available at our institution. In summary, Histoplasma capsulatum is a common pathogen that only rarely causes musculoskeletal infection, with isolated osteomyelitis being distinctly uncommon. Successful treatment presented in the literature involves debridement and long-term oral antifungal treatment, the first line being itraconazole. Long-term follow-up and collaboration with a pathologist and an infectious disease specialist are recommended.
Reference: McCabe MP, Heck RK. Histoplasma osteomyelitis simulating giant-cell tumor of the distal part of the radius. A case report. J Bone Joint Surg Am. 2010;92:708-14.
Giant-cell tumor of bone
Chondroblastoma
Fungal osteomyelitis
Tuberculous osteomyelitis




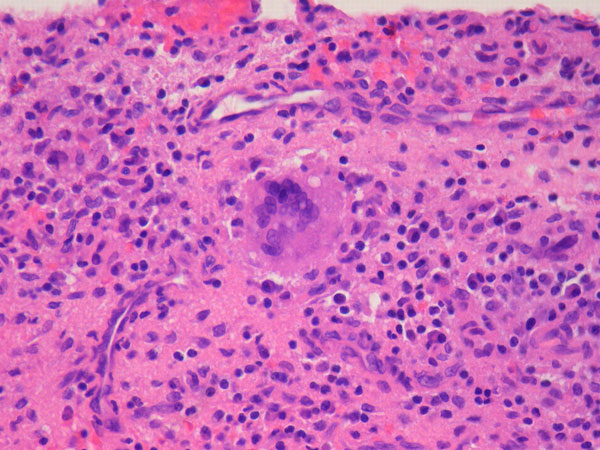

 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 1-C
Fig. 1-C Fig. 2-A
Fig. 2-A Fig. 3
Fig. 3 Fig. 2-B
Fig. 2-B Fig. 4-A
Fig. 4-A Fig. 4-B
Fig. 4-B