A thirty-three-year-old right-hand-dominant man who worked as an inventory manager was referred to us after being treated for progressive loss of motion following a hyperextension injury. The primary care physician had performed the initial evaluation and treatment four months after the injury. At that time, there had been lateral and anterior tenderness on clinical examination, without motion restriction. The patient was referred for physical therapy but gradually had development of activity-related pain and progressive loss of elbow motion that limited his ability to perform activities of daily life. The patient was referred to us nine months after the initial injury of the elbow. At that time, the patient complained of progressive loss of motion, pain along the medial aspect of the elbow, and intermittent paresthesias in the distribution of the ulnar nerve. The clinical examination revealed a healthy young man with an unremarkable medical history except for a previous problem with gastritis. The patient denied any constitutional symptoms such as night sweats, fever, weight loss, or any other systemic complaints. Aside from the involved elbow, the general physical examination was unremarkable. Examination of the right elbow revealed a flexion contracture of 40° and a 10° loss of flexion as compared with the left elbow. The patient had normal forearm rotation bilaterally. No evidence of active synovitis of the elbow was noted, no swelling was observed, and no masses were palpable. The ulnar nerve was tender to palpation, but no motor or sensory deficits were detected clinically. Routine anteroposterior and lateral radiographs of the elbow did not show any abnormality. An electromyographic study of the right upper extremity, performed because of symptoms of numbness and tenderness of the ulnar nerve, revealed unremarkable findings. In spite of vigorous physical therapy and the application of a turnbuckle splint, the elbow motion deteriorated to a 60° flexion contracture with active flexion to only 90°. The gallium scan revealed isolated gallium uptake only in the elbow. Magnetic resonance imaging showed a small joint effusion with a bone-marrow abnormality involving the distal metaphysis and epiphysis, with low T1 signal and high T2 signal and with patchy enhancement following the administration of gadolinium. There was also enhancement surrounding the ulnar nerve at the level of the cubital tunnel (Figs. 1-A, 1-B, 1-C). Because of the progressive impairment, an elbow exploration and capsulectomy was advised. With the patient under general anesthesia and with use of a sterile tourniquet, the elbow joint was approached through a straight posterior incision. A complete anterior and posterior capsulectomy was performed. A small amount of fleshy, tan tissue was observed in the olecranon fossa at the end of the procedure and was sent for permanent histopathological evaluation. Frozen-section analysis was not performed. The distal part of the humerus and the surrounding soft tissues were of normal macroscopic appearance. Full elbow extension was achieved at the end of the procedure. The histology of the soft-tissue lesion in the olecranon fossa is shown in Figures 2-A and 2-B.
Histological analysis of the tissue specimen revealed a diffuse infiltrate of large atypical lymphoid cells with oval, irregular, indented, or lobated nuclei; inconspicuous nucleoli; and scant cytoplasm. There also were areas of overlying hyperplastic synovium with chronic synovitis. Immunohistochemical stains showed that the atypical cells were CD20+ (B cells) and that many coexpressed CD10 and bcl-2. A stain for CD30 was negative, but many mixed small T cells (CD3+) were seen. These results confirmed the diagnosis of a diffuse large B-cell non-Hodgkin’s lymphoma with areas of chronic synovitis. There were no postoperative complications. Six weeks after surgery, the range of motion of the elbow had improved to 125° of flexion with a 10° flexion contracture. The patient was referred for treatment and a staging workup with elbow magnetic resonance imaging and computed tomographic scans as well as a gallium scan. The findings were consistent with the diagnosis of lymphoma. The patient met the criteria for stage-IAE diffuse large B-cell non-Hodgkin’s lymphoma of the right elbow and was managed with three courses of CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) chemotherapy followed by field radiation therapy. The humerus and the right elbow were treated with a total of 48.6 Gy with use of an anteroposterior/posteroanterior field technique with 6-MV photons over thirty-six consecutive days. At the time of the most recent follow-up, fifty-four months after treatment with chemotherapy and radiation therapy, the patient was in complete remission without evidence of recurrent disease. The patient had returned to his previous occupation and reported no limitation of his daily activities. There was an almost complete pain-free range of motion of the right elbow, with 125° of flexion on the right side as compared with 145° on the left side. There was full elbow extension and forearm rotation bilaterally.
Proceed to Discussion >>Reference: Jawa A, Lieberman AE, Alexieva CC, Jupiter JB. Primary intra-articular non-Hodgkin’s lymphoma of the elbow. A case report. J Bone Joint Surg Am. 2006 Dec;88(12):2730-4.
A review of the English-language literature revealed thirteen cases of non-Hodgkin’s lymphoma presenting in a joint and involving the synovium. The age of the patients ranged from thirteen to seventy-six years, with seven female and six male patients being affected. The knee was affected in eleven of the thirteen patients, whereas the wrist and sternoclavicular joint were involved in the remaining two. All patients presented with symptoms of pain, swelling, and decreased range of motion or systemic complaints. The association of non-Hodgkin’s lymphoma with immunosuppressive diseases is well established and was present in five of these patients. Five patients had no evidence of disease on plain radiographs, and additional imaging studies or procedures were needed for diagnosis. In one patient, malignant disease was only recognized after a total knee replacement had been performed. Chemotherapy and radiation therapy, in combination or individually, was used in all patients for whom treatment was recorded. The clinical outcome varied from complete remission and resolution of symptoms to death one month after diagnosis. However, those with a poor prognosis had either an associated immunosuppressive co-morbidity or were treated before the development of modern techniques of diagnosis and management. The typical workup for posttraumatic elbow stiffness involves radiographs to assess for deformity, heterotopic ossification, or fracture-healing. Sometimes, stress radiographs can provide additional assessment of instability. Additional imaging with computed tomography scanning is indicated to help assess complex osseous architecture in the setting of deformity, large osteophytes, and fracture-healing in order to help with surgical planning. Also, a magnetic resonance imaging scan is useful to assess medial and lateral collateral ligament integrity or focal articular cartilage damage. A full understanding of the pathology of the stiff elbow is necessary before proceeding to surgery. The case of our patient presented a challenging diagnostic problem not only because of the rarity of the condition but also because of the presentation of the disease without symptoms usually associated with a malignant condition. The absence of local signs of inflammation or swelling in a healthy young adult with normal radiographic findings did not suggest the necessity of additional imaging studies such as magnetic resonance imaging before surgery. In addition, the intraoperative findings were quite limited and therefore frozen-section analysis was not performed. Our patient had a good outcome, with complete remission and resolution of symptoms. Radiation therapy around or to a joint can be associated with complications such as fracture, contracture, chronic pain, edema, decreased muscle strength, and stiffness. However, a review of the literature indicates that doses of up to 65 Gy around joints, as in this case, usually are not associated with substantial long-term morbidity. Radiation to the lower extremity may be associated with worse functional outcomes than radiation to the upper extremity is, and radiation in combination with chemotherapy may be associated with more acute tissue injury than radiation alone is. Ultimately, the treatment of a malignant lesion in an extremity requires a high level of suspicion and a team approach. If there is a suspicion of a malignant lesion on the basis of symptoms, comorbidities, and plain radiographs, additional workup should include laboratory studies, magnetic resonance imaging, and computed tomography scans of the affected joint as well as additional staging studies, including bone scans and chest and abdominal computed tomography scans. A computed tomography-guided or open biopsy is typically indicated to make a definitive diagnosis. Furthermore, a team approach with orthopaedic, medical, and radiation oncologists as well as musculoskeletal radiologists and pathologists is essential for the proper care of the patient. In retrospect, our patient would have benefited from a more thorough workup of the elbow stiffness with preoperative magnetic resonance imaging and computed tomography scans. Additionally, if a change in diagnosis will influence intraoperative management, or if it is anticipated that fresh tissue may be required for special studies, then frozen-section analysis followed by evaluation of permanent histological sections should be performed.
Reference: Jawa A, Lieberman AE, Alexieva CC, Jupiter JB. Primary intra-articular non-Hodgkin’s lymphoma of the elbow. A case report. J Bone Joint Surg Am. 2006 Dec;88(12):2730-4.
Non-Hodgkin’s lymphoma
Lymphangioma
Lymph node enlargement associated with human immunodeficiency virus (HIV)
Hodgkin’s lymphoma
Lymphoproliferative disorder

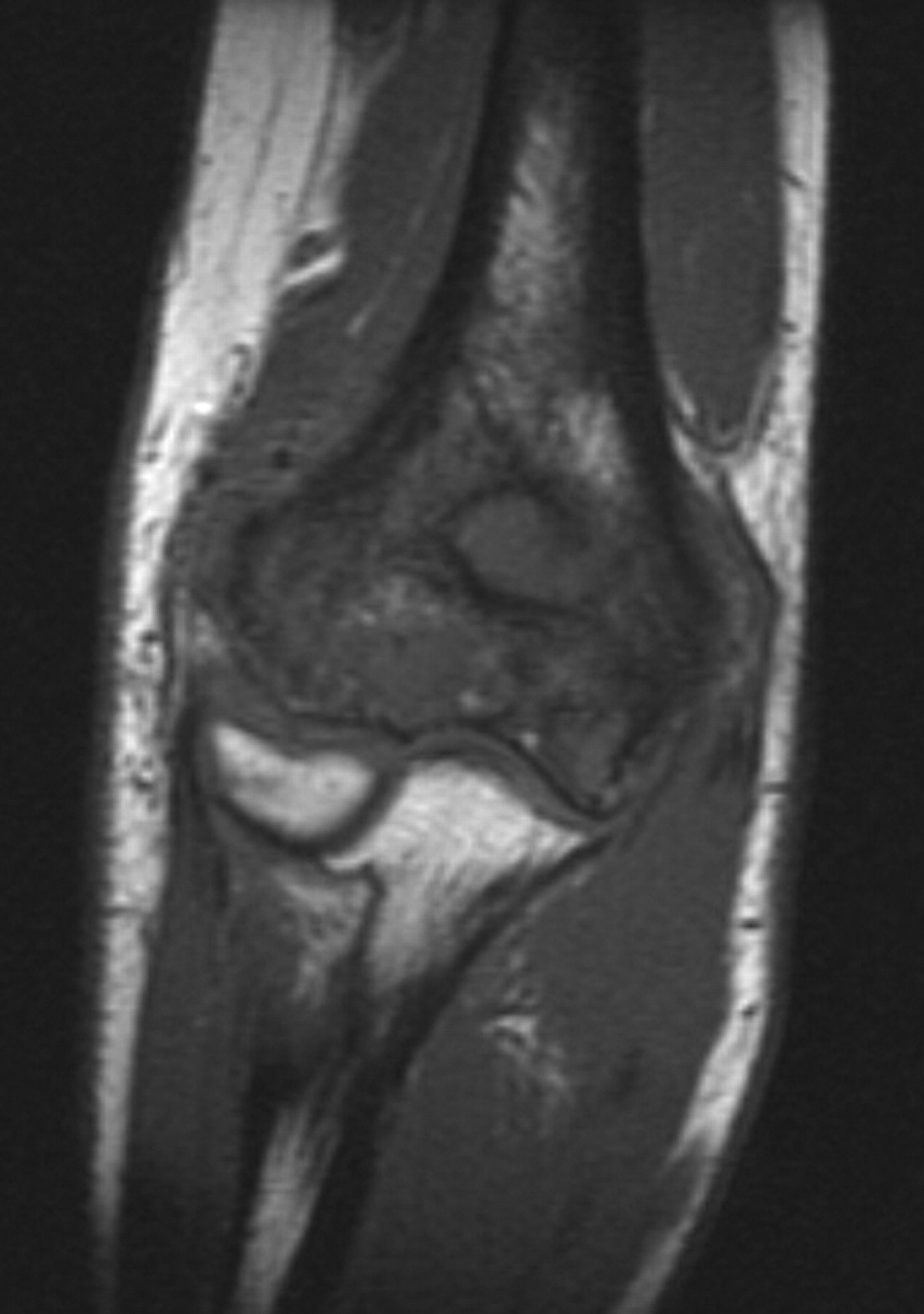
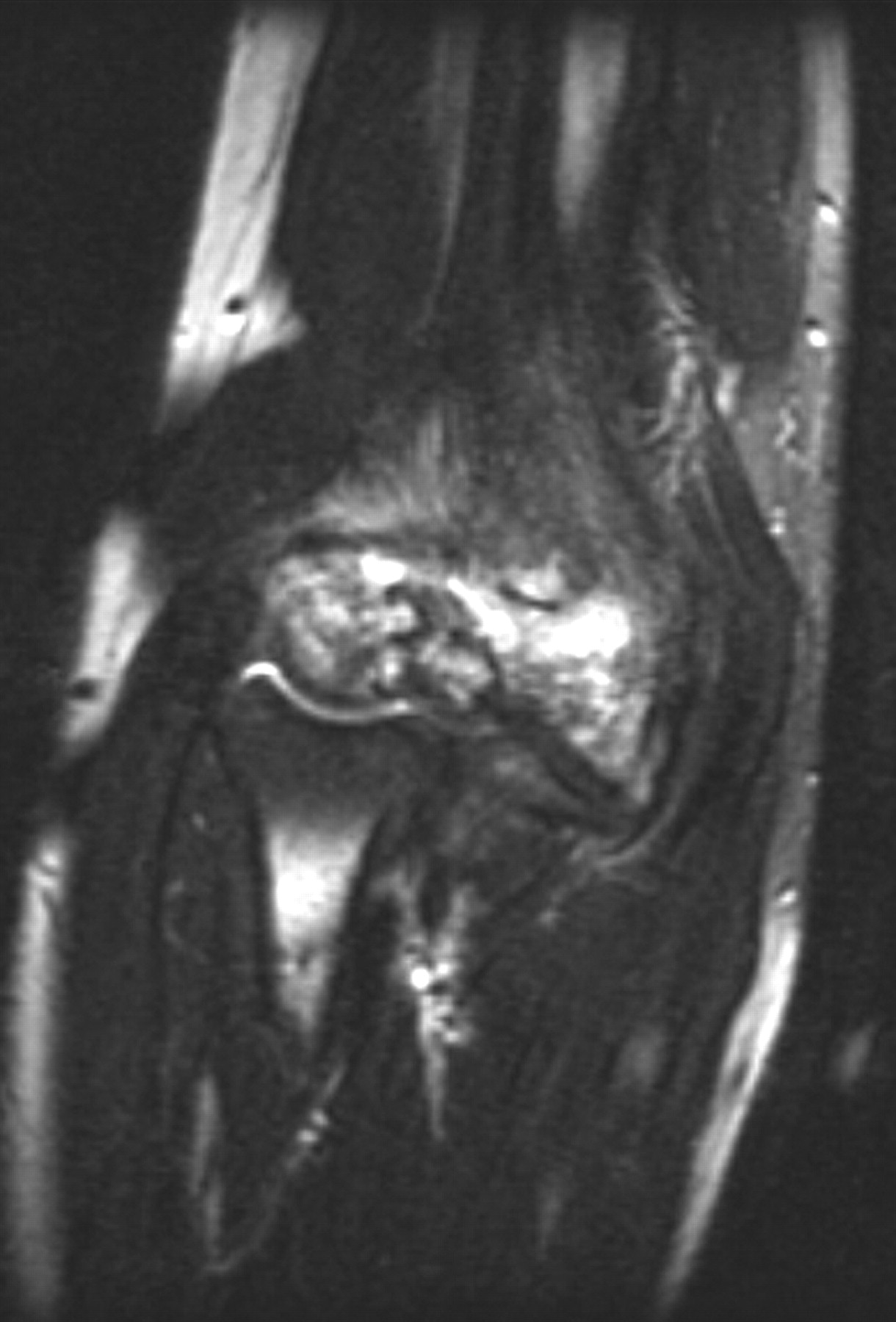
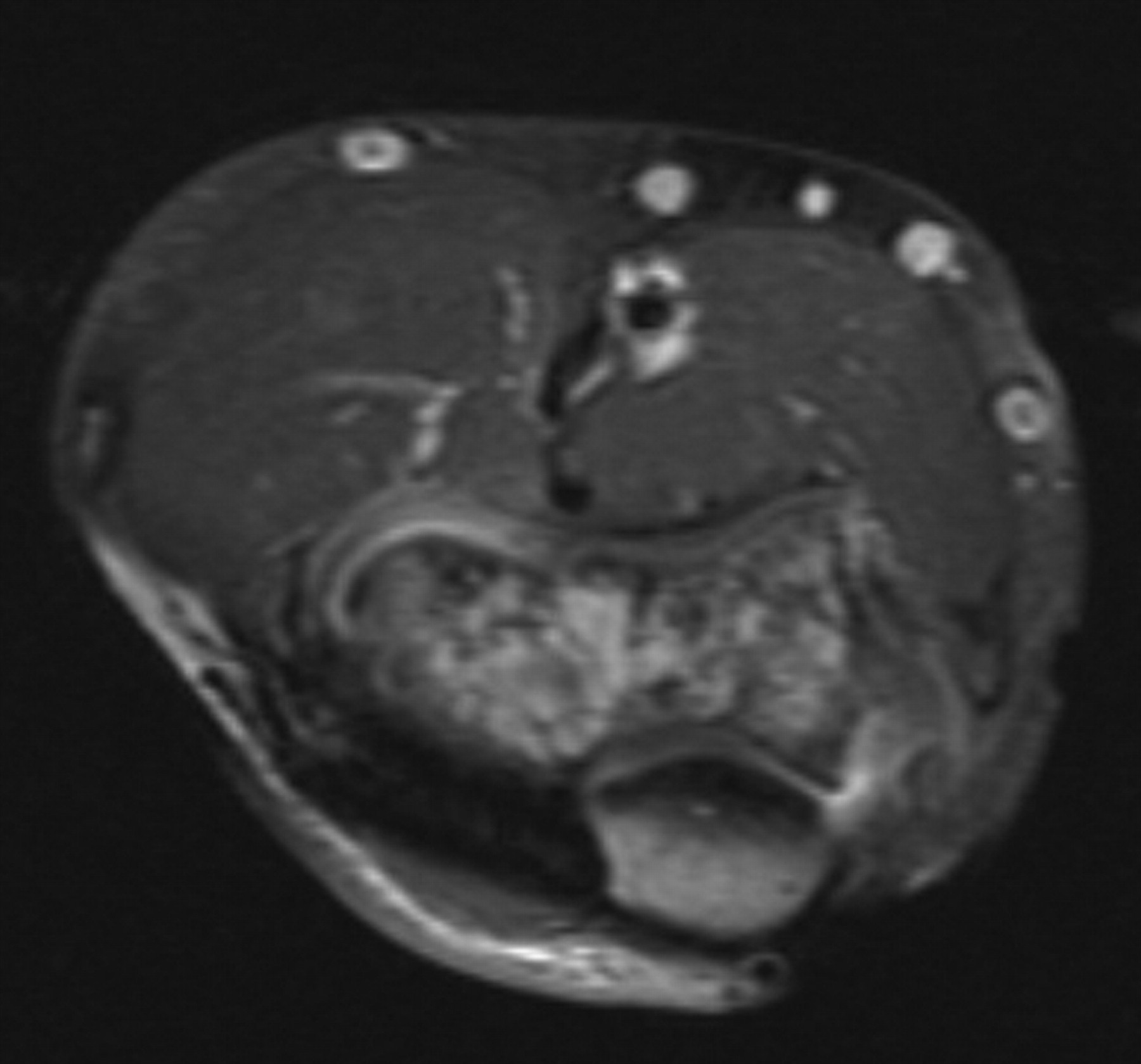
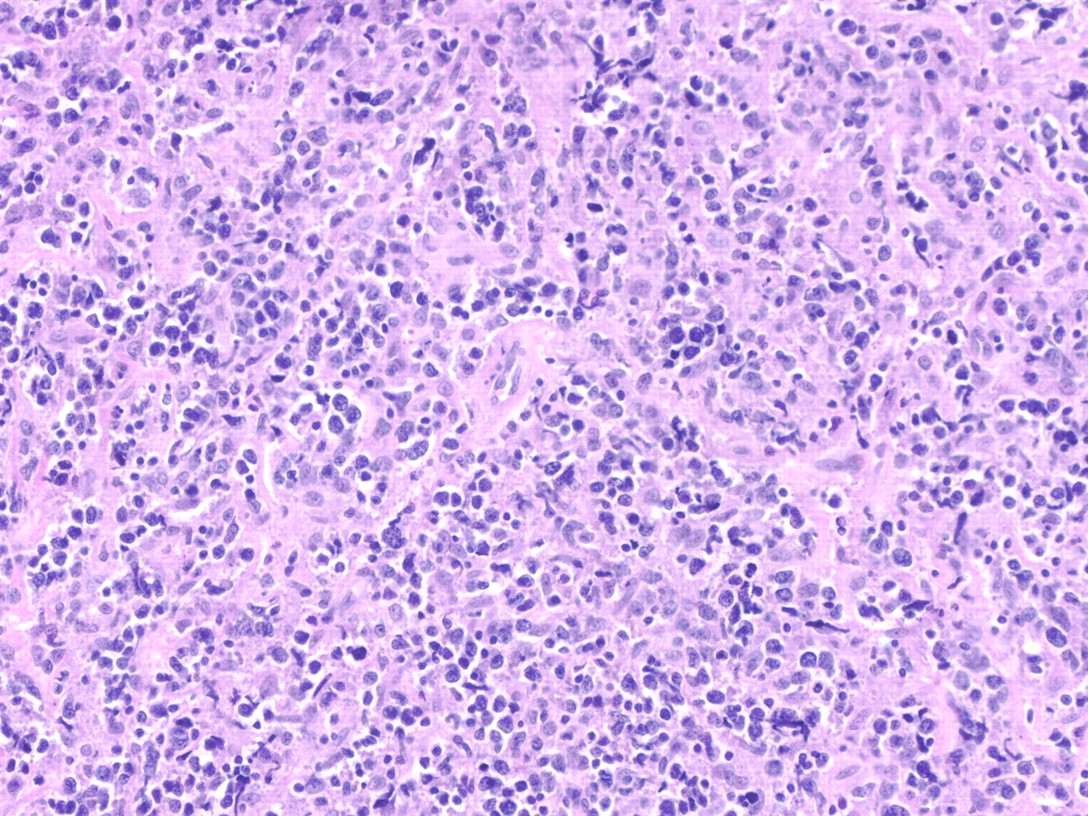

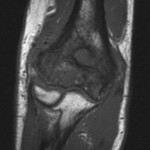 Fig. 1-A
Fig. 1-A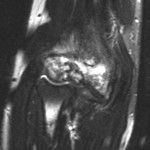 Fig. 1-B
Fig. 1-B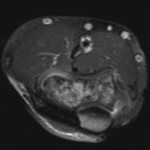 Fig. 1-C
Fig. 1-C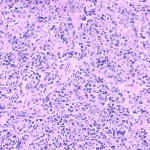 Fig. 2-A
Fig. 2-A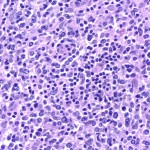 Fig. 2-B
Fig. 2-B