A Thirty-three-Year-Old Woman with Left Groin Pain
April 2, 2014
A thirty-three-year-old woman presented with a seven-week history of pain in the left groin. This had started with an episode that she described as a “give-away” sensation of the leg without any falls. Since then, she had experienced pain in the left groin radiating into the left thigh. There was no preceding trauma and she never had previously experienced this pain. A trial of anti-inflammatory drugs and physiotherapy had failed to ease the symptoms. On initial presentation, she had a reduced walking distance of fifty yards, and she experienced pain at rest and at night. Other medical problems included a long history of obesity, with a body weight of 111 kg, for which she had undergone gastric bypass surgery two years prior to presentation. She had since lost 24 kg, which reduced the body mass index from 43.3 to 34. On clinical examination, the Trendelenburg sign was positive on the left side. Tenderness was found anterior to the left hip joint but not over the greater trochanters. Range of motion of the left hip was restricted in all directions by pain. Radiographs of the pelvis and hips showed normal appearance of the pelvis, proximal part of the femora, and femoral heads; laboratory tests revealed an erythrocyte sedimentation rate (ESR) of 22 mm/h (normal range, <20 mm/h) and an alkaline phosphatase level of 144 IU/L (normal range, 30 to 130 IU/L).
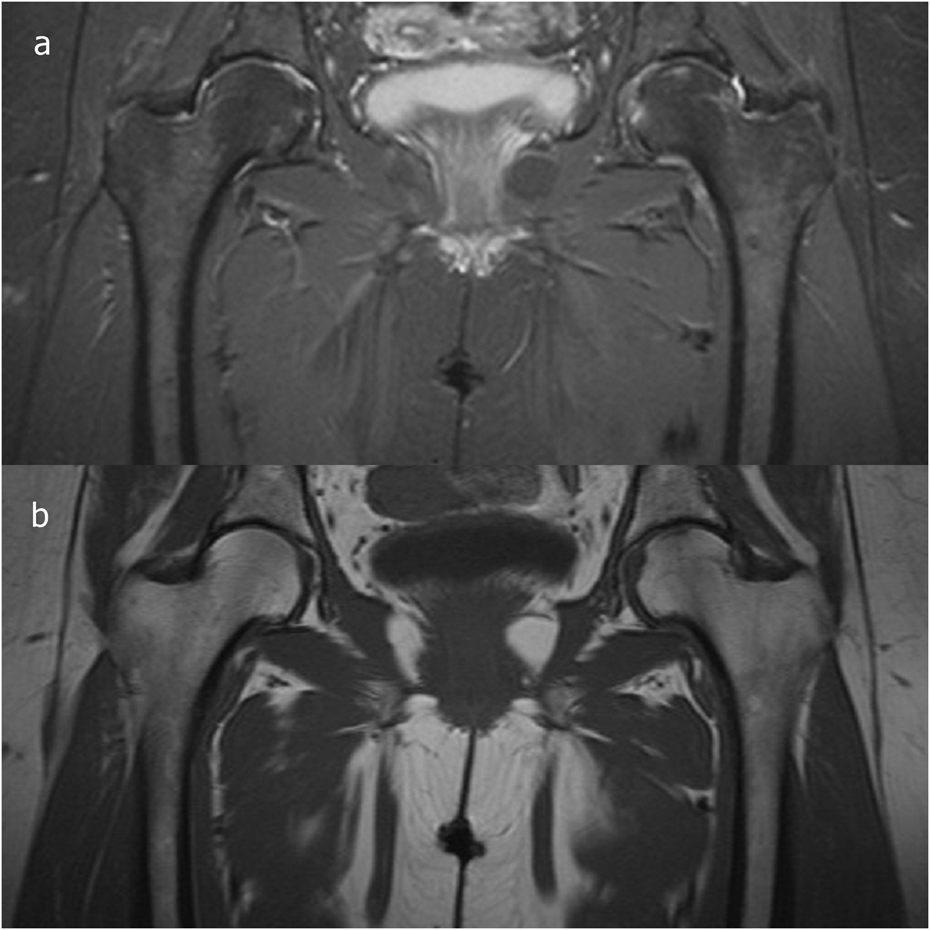
MRI of the pelvis demonstrated gross edema of the head and neck of the left femur, together with a small effusion in the hip joint (Figs. 1-A and 1-B). The patient subsequently underwent a whole-body bone scan, which demonstrated slightly increased uptake in the head of the left femur; she was diagnosed with bone marrow edema syndrome (BMES) of the left hip. Dual x-ray absorptiometry demonstrated decreased radiodensity with a young adult T-score of −1.4 of the left femoral neck. The T-score was slightly reduced but still within normal range in the rest of the skeleton, −0.4 in the contralateral femoral neck, and −0.2 in the lumbar spine. For management of the BMES, the patient was advised to keep the left leg non-weight-bearing, and she was started on calcium and vitamin D supplements. After three months, the symptoms had started to subside, and she was able to walk without aids. A repeat MRI confirmed resolution of the signs of BMES (Figs. 2-A and 2-B).
Proceed to Discussion >>Reference: Siebachmeyer M, Fenton P, Rai HS, Selzer G. Bone marrow edema syndrome of the proximal part of the femur following gastric bypass surgery: a case report. JBJS Case Connector. 2014 Feb 12;4(1):e15 1-4.
BMES, also known as transient osteoporosis, is a self-limiting, reversible disease of uncertain etiology. It presents with pain and usually involves the femoral head and neck, but can also occur in the knees or ankles. It typically affects middle-aged men, women in the last trimester of pregnancy, or postpartum women. It is a diagnosis of exclusion since bone marrow edema can also accompany stress fractures, traumatic bone-bruising, osteonecrosis, osteochondritis dissecans, degenerative processes (including arthrosis and rapid destructive osteoarthritis), osteomyelitis, and neoplasms. The histological appearance of transient osteoporosis of the hip has been described as thin and disconnected bone trabeculae covered by osteoid seams and active osteoblasts. The bone marrow is edematous with associated vascular congestion. Diagnosis of BMES is based on history and clinical examination. Laboratory tests may reveal only a mildly raised ESR and alkaline phosphatase level. Radiographs should be the first-line imaging for investigating hip pain, but radiographic manifestation may not develop for up to one month after the onset of symptoms. MRI is the most sensitive and specific imaging modality for detecting bone marrow edema and excluding many other differential diagnoses. Pathological changes may manifest within a few days, with extensive bone marrow edema-like signal in the affected region with possible joint effusion. It can be distinguished from osteonecrosis by the absence of subchondral lesions. Osteonecrosis of the femoral head is a related disease that is progressive and is characterized by focal subchondral low signal intensity lesions in T1-weighted sequences and a pathognomonic double-line sign in T2-weighted sequences. In later stages, radiographs may demonstrate areas of central lucency with a sclerotic border or signs of subchondral collapse. In contrast, BMES not only affects the epiphysis, but can extend into the metaphysis or even the diaphysis of a long bone. There is ongoing debate in the literature as to whether BMES represents the initial stage of osteonecrosis or whether the two conditions are separate entities. The latter is supported by radiographic and histopathological studies, but the similarities of the two conditions, especially in their initial stages, are well described. Hofmann et al. described the role of abnormal microcirculation within the subchondral bone in the pathogenesis of osteonecrosis. With use of the Association Research Circulation Osseous (ARCO) classification, they classified BMES as a variant of the early stage (ARCO I) of the five stages of osteonecrosis. At this stage, osteonecrosis may result in complete restoration of the bone structure; therefore, it is called the “early reversible stage.” The principles of treatment of BMES are pain relief and prevention of trabecular microfractures. Regression of symptoms occurs within a few months to one year. During the acute phase, resting of the joint is advised, and walking with aids can reduce biomechanical stress at the lesion with the benefits of pain relief and fracture prevention. Physiotherapy with range-of-motion exercises can help to prevent stiffness of the joint and to aid protected weight-bearing. In addition to symptomatic treatment with analgesics and nonsteroidal anti-inflammatory drugs, calcium and vitamin D3 supplements have been recommended to accelerate recovery. Other pharmacological approaches have been tried, including intravenous bisphosphonates (ibandronate) and calcitonin, but the evidence is limited because of the small number of cases and the self-limiting nature of the condition. One study demonstrated good pain relief following administration of iloprost, a prostacyclin analogue. Because of its effects on the terminal vascular bed, including vasodilatation and reduction of capillary permeability, it was suggested that prostacyclin represents a more causative treatment approach and may even play a curative role in the early stage of osteonecrosis and BMES. Other studies report good pain relief from surgical approaches, suggesting that the duration of symptoms could be decreased by core decompression to relieve bone marrow pressure. Proper nutrition is essential for normal growth and good bone quality. Calcium is the specific nutrient that is most important for preventing and treating osteoporosis. The recommended calcium intake for adults is 1000 to 1500 mg per day. Optimal calcium absorption depends on vitamin D, which is therefore important for bone health. The efficiency of calcium absorption is affected by calcium availability, calcium and vitamin D status of the body, growth, pregnancy, lactation, and old age. It is also dependent on an acid intraluminal environment and the presence of calcium-binding protein, both of which can be found in the duodenum and proximal part of the jejunum. The relation between calcium and vitamin D insufficiency as a risk factor for the development of osteoporosis is widely recognized, but its role in the etiology of transient osteoporosis is unclear, especially since transient osteoporosis affects a different population, including young pregnant women; other theories of etiology exist, such as the concept of venous congestion during pregnancy. More recent studies have established a relation between bariatric surgery and osteoporosis. It has been demonstrated that patients may develop secondary hyperparathyroidism with increased bone resorption following gastric bypass surgery. This, in turn, may lead to bone loss and increased fracture risk. In our case, the patient had undergone gastric bypass surgery two years before the onset of the transient osteoporosis. Unfortunately, the parathyroid hormone levels had not been tested when she initially had presented. At that time, surgery-induced calcium insufficiency or secondary hyperparathyroidism as causative factors of the transient osteoporosis were not proven. The known effects of obesity-surgery-induced malabsorption states on bone metabolism could suggest the hypothesis of a link between gastric bypass surgery and the onset of BMES in our patient. On the other hand, a possibly weakened skeleton may have been more susceptible to bone-bruising following trauma, as described by our patient as a “give-away” event of the leg. Additional biochemical tests, including parathyroid hormone levels, in future cases would be helpful to investigate the role of calcium and vitamin D insufficiency in transient osteoporosis. In summary, BMES is rare and its etiology is unclear. Some studies suggest that it is a separate entity from osteonecrosis. The role of calcium and vitamin D in the genesis and treatment of osteoporosis is recognized, and their therapeutic effect in the recovery of the femoral head from BMES makes sense. Our case suggests the possible implication of gastric bypass in the development of transient osteoporosis, which should be subject to additional studies and investigation.
Reference: Siebachmeyer M, Fenton P, Rai HS, Selzer G. Bone marrow edema syndrome of the proximal part of the femur following gastric bypass surgery: a case report. JBJS Case Connector. 2014 Feb 12;4(1):e15 1-4.
Lymphoma of the proximal femur
Acetabular labral tear
Bone marrow edema syndrome
Femoral neck stress fracture
Osteonecrosis of the femoral head

 Fig. 1
Fig. 1 Fig. 2
Fig. 2