A Twenty-one-Year-Old Woman with Ankle Swelling and Pain
October 19, 2011
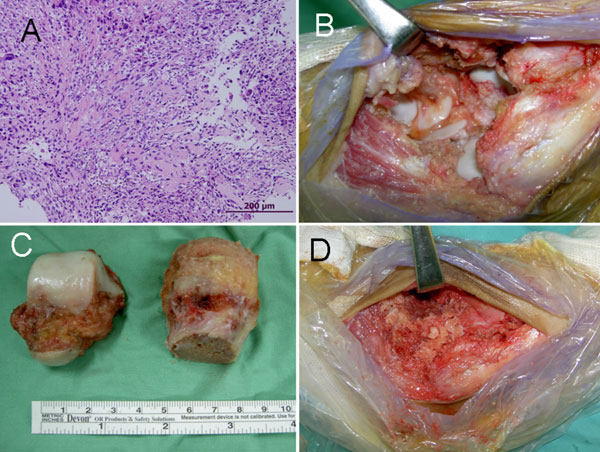
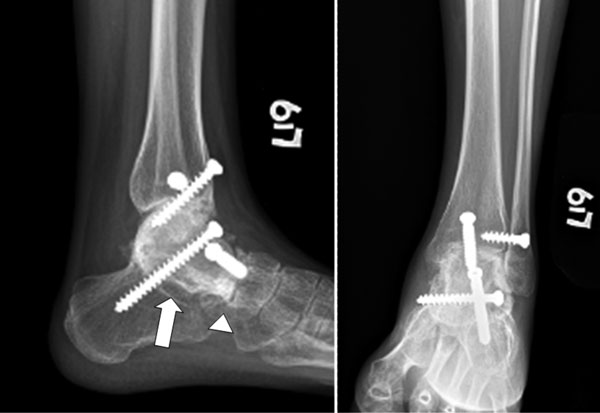
A twenty-one-year-old woman presented in July 2008 with a six-month history of swelling and discomfort in the left ankle. She recalled no history of trauma. Physical examination revealed slight swelling and a limited range of motion of the left ankle. All laboratory data were within normal limits, except for mild elevation of the C-reactive protein level (0.98 mg/dL; normal, <0.8 mg/dL). Plain radiographs showed a geographic osteolytic lesion with a sclerotic margin involving the medial portion of the left talus (Fig. 1). Magnetic resonance imaging (MRI) revealed a 4 × 1.8 × 3.3-cm geographic destructive osseous lesion with a sclerotic margin in the talus, and adjacent soft-tissue edema with fluid accumulation in both the talotibial and the talonavicular joint. The signal intensity was intermediate to high on the T1-weighted (fast-spin-echo) images and high on the T1-weighted (fat-suppressed) images with good contrast enhancement (Fig. 2). Technetium-99m-methylene diphosphonate (Tc-99m-MDP) scintigraphy showed a persistent focal tracer uptake in the left ankle, and a thallium-201 whole body scan also revealed an intense focal tracer uptake at the same location. Computed tomography (CT) of the chest showed no definite focal lesions. Open incisional biopsy of the talar lesion was performed. Histology is seen in Figure 3.
Histologic examination showed sheets of highly anaplastic tumor cells with hyperchromatic nuclei and malignant osteoid production, findings compatible with a diagnosis of conventional osteosarcoma (Fig. 4-A). The patient then underwent neoadjuvant chemotherapy with three courses of cisplatin and doxorubicin. Three months after the open biopsy, an MRI study showed no progression of the malignant tumor, and repeated Tc-99m-MDP scintigraphy revealed a small, persistent hot area involving the distal part of the left tibia. A marginal resection of the left talus was performed (Fig. 4-B). All of the articular surfaces of the talus were intact, and the bone surfaces were irregular with attached soft tissue (Fig. 4-C). No extraosseous tumor invasion was noted at the time of the operation. We removed the articular cartilage of the ankle mortise, the talonavicular joint, and the subtalar joint to expose cancellous bone for arthrodesis. An allogenic bone graft from a femoral head was sculpted to fit the size and shape of the excised talus (Fig. 4-C). The bone graft had been harvested during a hip arthroplasty under strictly aseptic technique and had been frozen at ˗70°C before implantation. After removal of the left talus, the defect was reconstructed with the bone graft (Fig. 4-D). We completed the arthrodesis by inserting three cancellous compression screws across the tibiotalar, subtalar, and talonavicular joints. Morselized bone chips were used to fill any gaps between the prepared bone graft and the ankle mortise. Histopathologic examination showed an osteosarcoma with resection margins free of tumor, although the tumor had penetrated through the cortex into the adjacent soft tissue. The overall tumor necrosis rate was >95%. The surgical stage was IIB according to the Musculoskeletal Tumor Society (MSTS) staging system, and T1N0M0, stage IIA, according to the American Joint Committee on Cancer (AJCC) staging system. Postoperatively, the patient underwent adjuvant chemotherapy with one more course of cisplatin and doxorubicin. Follow-up radiographs made nineteen months after the operation showed successful osseous fusion across the tibiotalar, subtalar, and talonavicular joints (Fig. 5). CT demonstrated integration between the allogenic bone graft and the calcaneus and navicular. The patient could walk without an orthosis, and there was no evidence of local recurrence. The functional scores according to the MSTS and the Toronto Extremity Salvage Score (TESS) were 86% and 89.5 points, respectively.
Proceed to Discussion >>Reference: Wang CW, Chen CY, Yang RS. Talar osteosarcoma treated with limb-sparing surgery. A case report. J Bone Joint Surg Am. 2011;93:e22(1-5).
The reported incidence of osteosarcoma of the foot is very low. In one series, only twelve (0.6%) of 1929 cases of osteosarcoma were in the bones of the foot. Biscaglia et al. noted that, in contrast to the typical osteosarcoma involving the long bones, which usually affects children and adolescents, osteosarcomas of the foot were seen almost exclusively in adults. In addition, compared with osteosarcomas elsewhere, osteosarcomas in the foot are more likely to be low-grade, and survival rates for patients with osteosarcoma of the foot are higher than those associated with osteosarcomas in general. Since Amini and Colacecchi first reported an osteosarcoma of the talus in 1980, there have been only seven case reports on osteosarcoma of the talus and nine cases of osteosarcoma of the talus in two case series of osteosarcomas in the foot. The symptoms are nonspecific pain and swelling, and the diagnosis is usually delayed. The typical radiographic features of periosteal reaction, such as a Codman triangle and a sunburst appearance, may not be present in osteosarcomas below the ankle. One study indicated that osteosarcomas localized to the calcaneus, tarsus, and talus are more commonly densely sclerotic lesions with ill-defined borders and extracompartmental bone production. Since the radiographic features may mimic various benign and malignant processes, other imaging studies, such as MRI, whole body scintigraphy, and open biopsy, should be performed to confirm the diagnosis. Patients with osteosarcoma of the foot have not usually been considered candidates for limb-sparing surgery. Amputation has been the standard treatment for the past several decades. However, below-the-knee amputation has many drawbacks, such as the need for the patient to depend on a prosthetic limb, phantom-limb pain, and chronic episodes of skin breakdown. Quan et al. examined twenty-seven patients with osteosarcoma near a joint and found no evidence of penetration across articular cartilage into the joint cavities. It was postulated that hyaline cartilage acts as a relative barrier and thus intra-articular resection may be safe. Furthermore, recent advances in imaging studies and chemotherapy can assist in the early detection and control of the local disease. With accurate imaging, a good response to preoperative chemotherapy, and improving limb-salvage techniques, some individuals may undergo limb-sparing surgery with acceptable outcomes. Katagiri et al. reported the first case of osteosarcoma of the talus treated successfully with a limb-sparing ankle arthrodesis. The functional outcomes measured with the MSTS and the TESS were 90% and 89 points, respectively, forty-seven months after the surgery. According to our review of the literature, only one patient in the series reported by Renard et al. and one in the study by Hopyan et al. were treated with below-the-knee amputation for osteosarcoma in the foot and ankle. The MSTS scores of these two patients were 60% and 70%, respectively. Davis et al. quantified the differences in physical disability of patients with lower-extremity sarcoma who had undergone amputation or limb-sparing surgery and found mean TESS scores of 75.6 and 85.7 points, respectively. In our patient, the MSTS score was 86% and the TESS score was 89.5 points at nineteen months after the surgery. In both our case and the case reported by Katagiri et al., the functional outcome of limb-sparing surgery was more favorable than that of traditional below-the-knee amputation.
Reference: Wang CW, Chen CY, Yang RS. Talar osteosarcoma treated with limb-sparing surgery. A case report. J Bone Joint Surg Am. 2011;93:e22(1-5).
Ewing sarcoma
Osteosarcoma
Fibrous dysplasia
Giant cell tumor


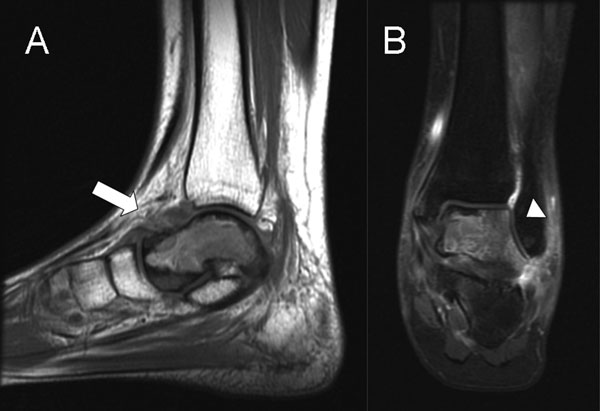
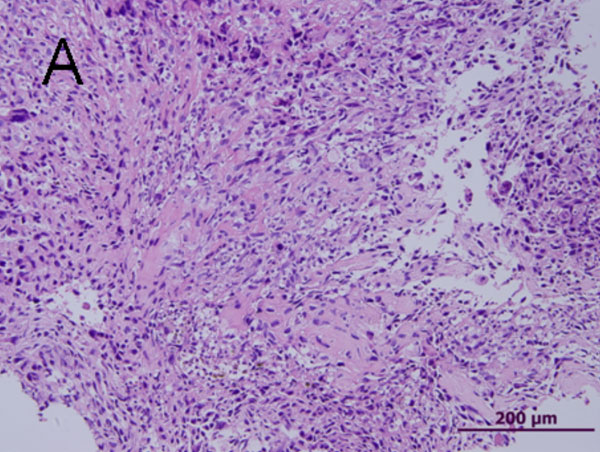
 Fig. 1
Fig. 1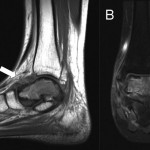 Fig. 2
Fig. 2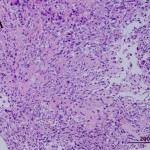 Fig. 3
Fig. 3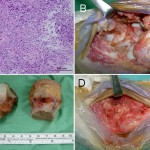 Fig. 4
Fig. 4 Fig. 5
Fig. 5