An Eighteen-Year-Old Baseball Pitcher with Shoulder Pain
July 16, 2014
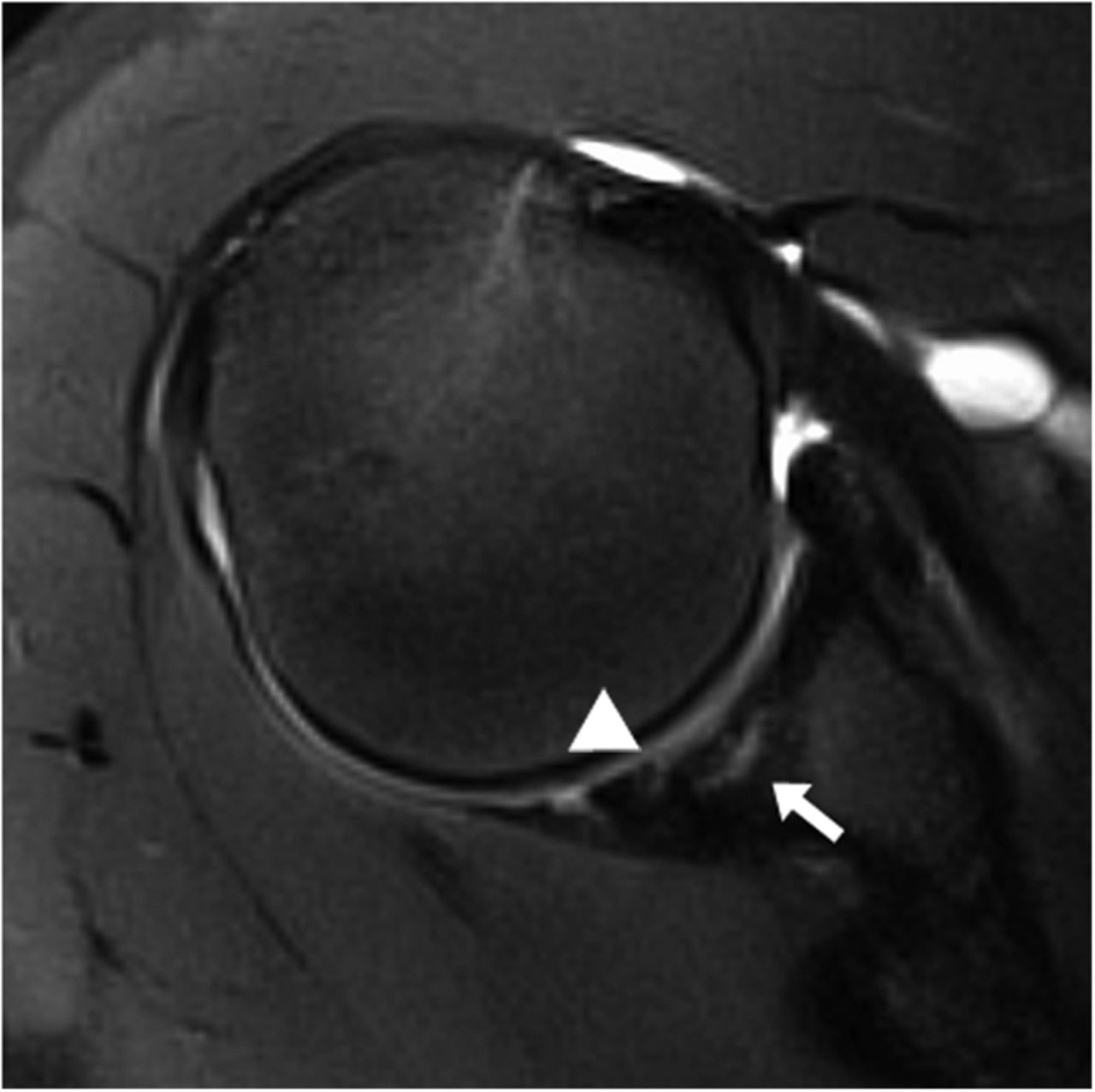
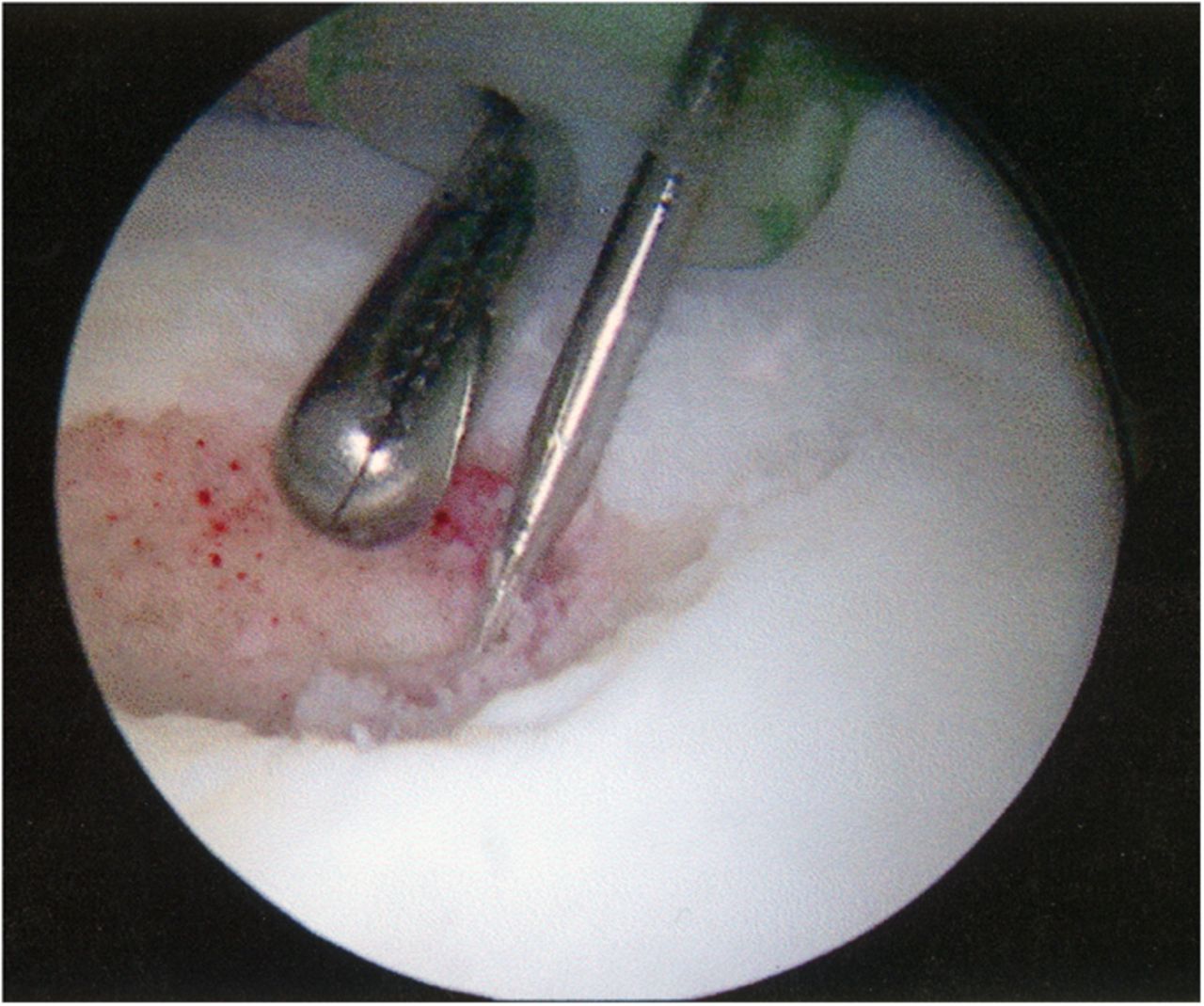
An eighteen-year-old right-hand-dominant baseball pitcher presented with a three-week history of pitching-related shoulder pain. He had also noticed decreased pitching velocity. He had been participating in physical therapy with the team trainer, but he had not had any improvement. Of note, the history included the diagnosis of Little League shoulder six years prior to evaluation. This had been treated with rest and a gradual return to play. He had been symptom-free until the current season. On physical examination, the patient demonstrated full active forward elevation and abduction. Rotator cuff strength testing was pain-free and symmetric to the contralateral side. Shoulder passive range of motion demonstrated symmetry except for 80° of internal rotation with the shoulder in 90° of abduction (20° to 30° less than the contralateral side), as well as 110° of external rotation with the arm in 90° of abduction (20° to 30° greater than the contralateral side). Biceps provocative tests were positive. Evaluation with radiographs, including anteroposterior, Grashey, scapular Y, and axillary views, was normal. The diagnosis of a probable superior labral anterior-posterior (SLAP) tear with a tight posterior capsule was made. The patient was sent for diagnostic magnetic resonance imaging (MRI) and continued with physical therapy. At the three week follow-up, the symptoms were still present, and MRI revealed increased signal on T2-weighted imaging in the subchondral bone in the posterior glenoid, as well as a small break in the cartilage on T1-weighted imaging (Fig. 1, Fig. 2, and Fig. 3).
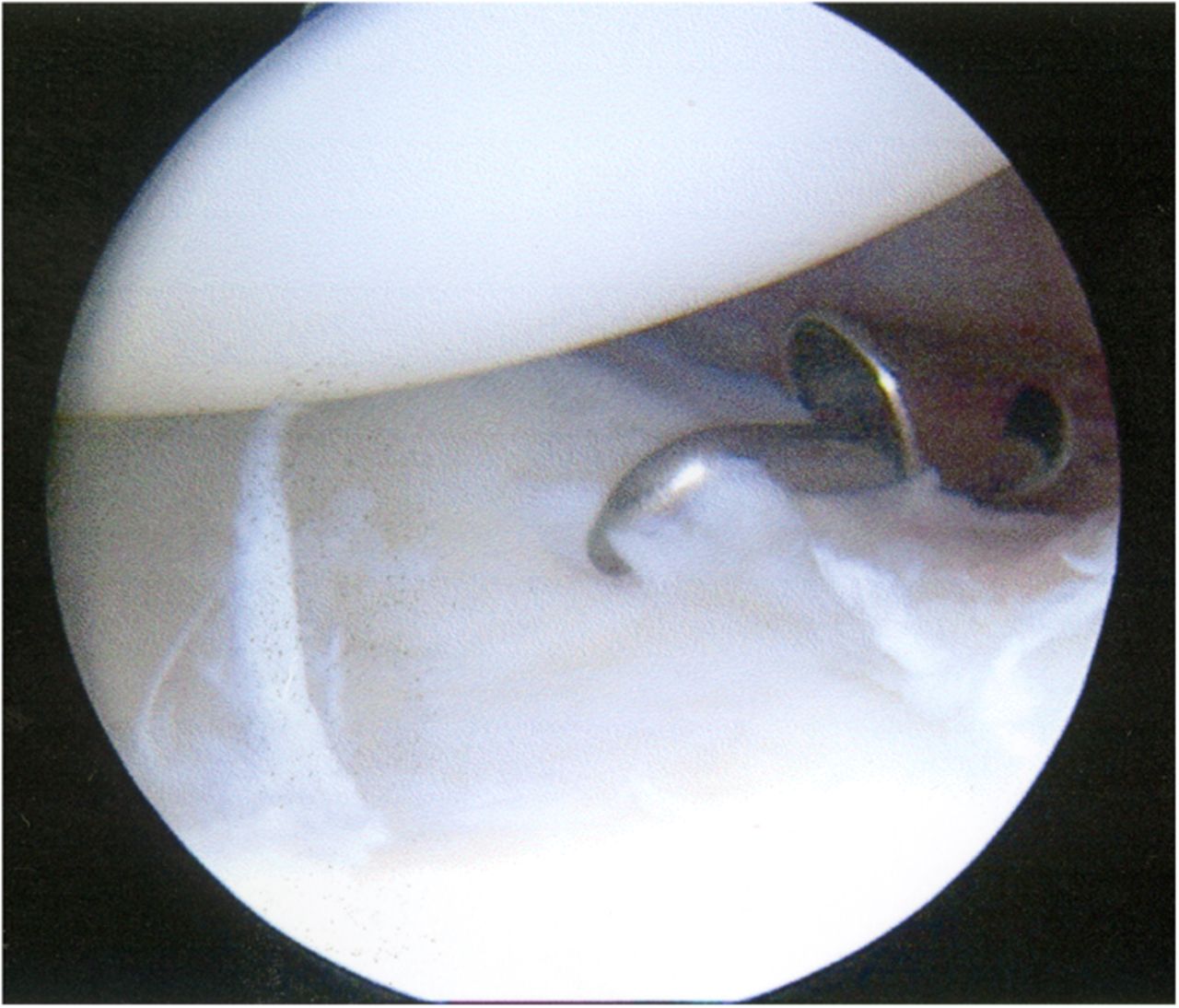
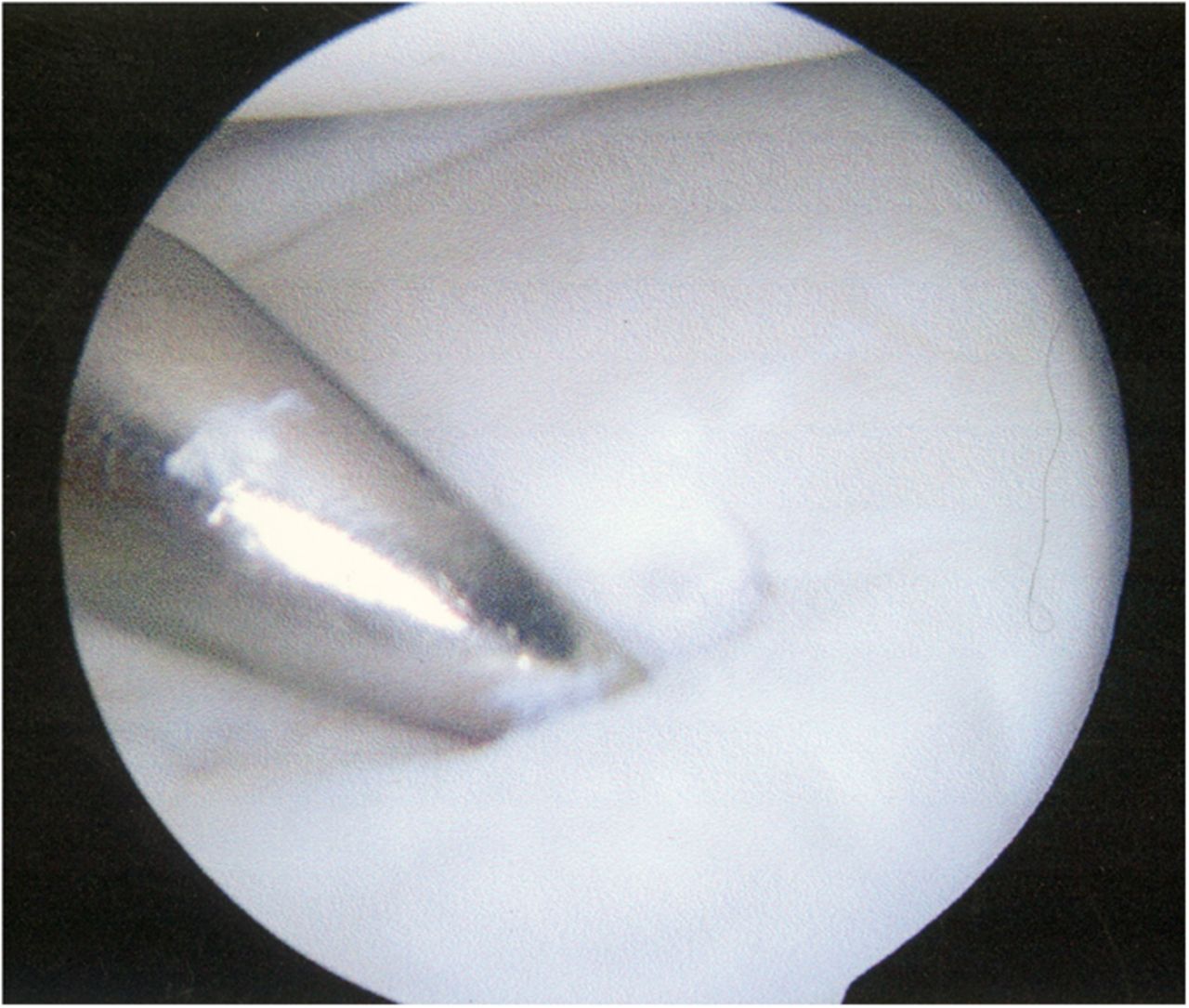
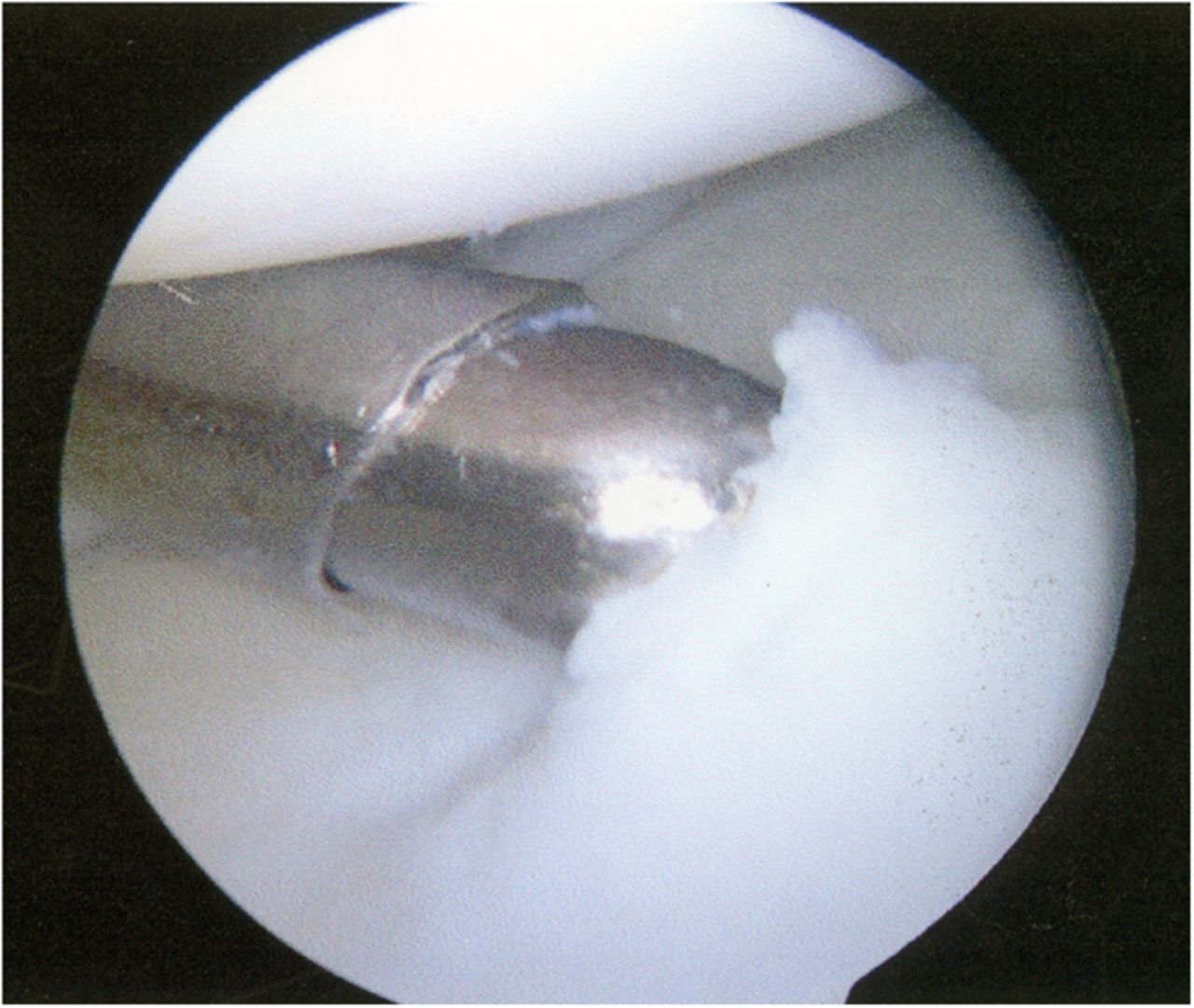
A Dipaola grade-2 adult osteochondritis dissecans (AOCD) lesion of the glenoid was the final diagnosis. Consent was obtained for an arthroscopic evaluation and possible microfracture surgery. Intraoperatively, while probing from anterior to posterior along the cartilage surface, a defect was identified (Fig. 4). Probing the cartilage overlying that area resulted in a “bounce,” indicating subchondral bone instability. An arthroscopic shaver and a biter were used to remove the lesion until there was exposed subchondral bone (measuring approximately 15 mm by 10 mm in diameter and 7 mm in depth). The subchondral bone was subsequently drilled to facilitate mesenchymal stem cell access (Figs. 5-A through 5-E). Postoperatively, the arm was placed in a sling, and the patient was instructed not to lift with the right arm. Physical therapy included passive range of motion and pendulum exercises for six weeks. The three-month follow-up examination revealed symmetrical painless range of motion. The patient was advanced to full activities beneath shoulder level. At the six-month follow-up, he was released and was able to return to competition. At nineteen months, he continued to report painless full range of motion. He has since transferred schools and no longer plays baseball collegiately for personal reasons, but he plays softball recreationally at a high level. He changed positions from pitcher to shortstop, and he has not experienced any functional limitations during competition. Although the shoulder has not been tested throughout the rigors of a collegiate season, the patient subjectively believes he could compete at a collegiate level without limitation.
Proceed to Discussion >>Reference: Coats A, Blomquist G, Kluemper CT, Ireland ML. An osteochondritis dissecans lesion of the glenoid in an adult: a case report. JBJS Case Connector. 2014 May 14;4(2):e37.
OCD of the glenoid is rare, and, to the best of our knowledge, only a few cases previously have been reported. Gogus and Ozturk described a lesion with glenoid cartilage loss and subchondral cyst formation that was treated with microfracture surgery. Chu et al. described a patient with a glenoid cartilaginous flap with mild subchondral bone edema that was treated with arthroscopic drilling. OCD lesions are classically situated on convex surfaces. Evaluation of these areas is best performed with diagnostic MRI. Dipaola’s grading scale has four grades based on MRI findings. In grade-1 lesions, there is thickening but no break in the articular cartilage. Grade-2 lesions do have an articular cartilage breach, with a mildly increased signal rim behind the fragment on T2-weighted imaging; this signal is suggestive of fibrous tissue attachment. Grade-3 lesions also have a breach in the articular cartilage, but with a high signal behind the fragment on T2-weighted imaging, suggesting the presence of joint fluid. Grade-4 lesions occur when the OCD becomes a loose body in the joint. When evaluating stability of a lesion, grades 1 and 2 are considered stable, while grades 3 and 4 are unstable. De Smet et al. found that 72% of OCD lesions with increased subchondral bone signal (grade 3) on T2-weighted imaging were unstable. According to this classification scheme, our patient had a grade-2 AOCD lesion. Intraoperative classification of OCD lesions most commonly uses the Guhl classification system. Grade-I lesions have cartilage irregularity and softening without any fissuring or definable fragment. Grade-II lesions have an articular cartilage breach without displacement of the lesion. Grade-III lesions have a definable fragment that is displaceable but still attached partially by some cartilage (flap lesion). Grade-IV lesions involve a loose body with the corresponding defect in the articular surface. Based on this classification, our patient’s lesion was consistent with a Guhl grade-III lesion because it was unstable but attached by the overlying cartilage. Compared with the juvenile form, AOCD lesions are less likely to heal, and their prolonged course typically results in lesion instability. For this reason, early aggressive surgical treatment is preferred. In our patient, the lesion had preoperative findings suggestive of a Dipaola grade-2 lesion. However, intraoperatively, the lesion displayed a more unstable pattern (Guhl grade-III lesion). In conclusion, our case demonstrates a rare OCD lesion of the glenoid in a concave non-weight-bearing joint. We attribute repetitive throwing motion as a contributing factor toward the formation of this lesion in an unusual location. With few reports in the literature, this case heightens awareness of this condition. We have presented one example of a good intermediate-term functional outcome in a young adult baseball player. More cases are needed to establish a prognosis for returning to competitive throwing sports.
Reference: Coats A, Blomquist G, Kluemper CT, Ireland ML. An osteochondritis dissecans lesion of the glenoid in an adult: a case report. JBJS Case Connector. 2014 May 14;4(2):e37.
Superior labral anterior-posterior (SLAP) lesion
Unstable glenoid rim fracture
Osteochondritis dissecans of the glenoid
Intra-articular chondroma
Anterior Bankart lesion



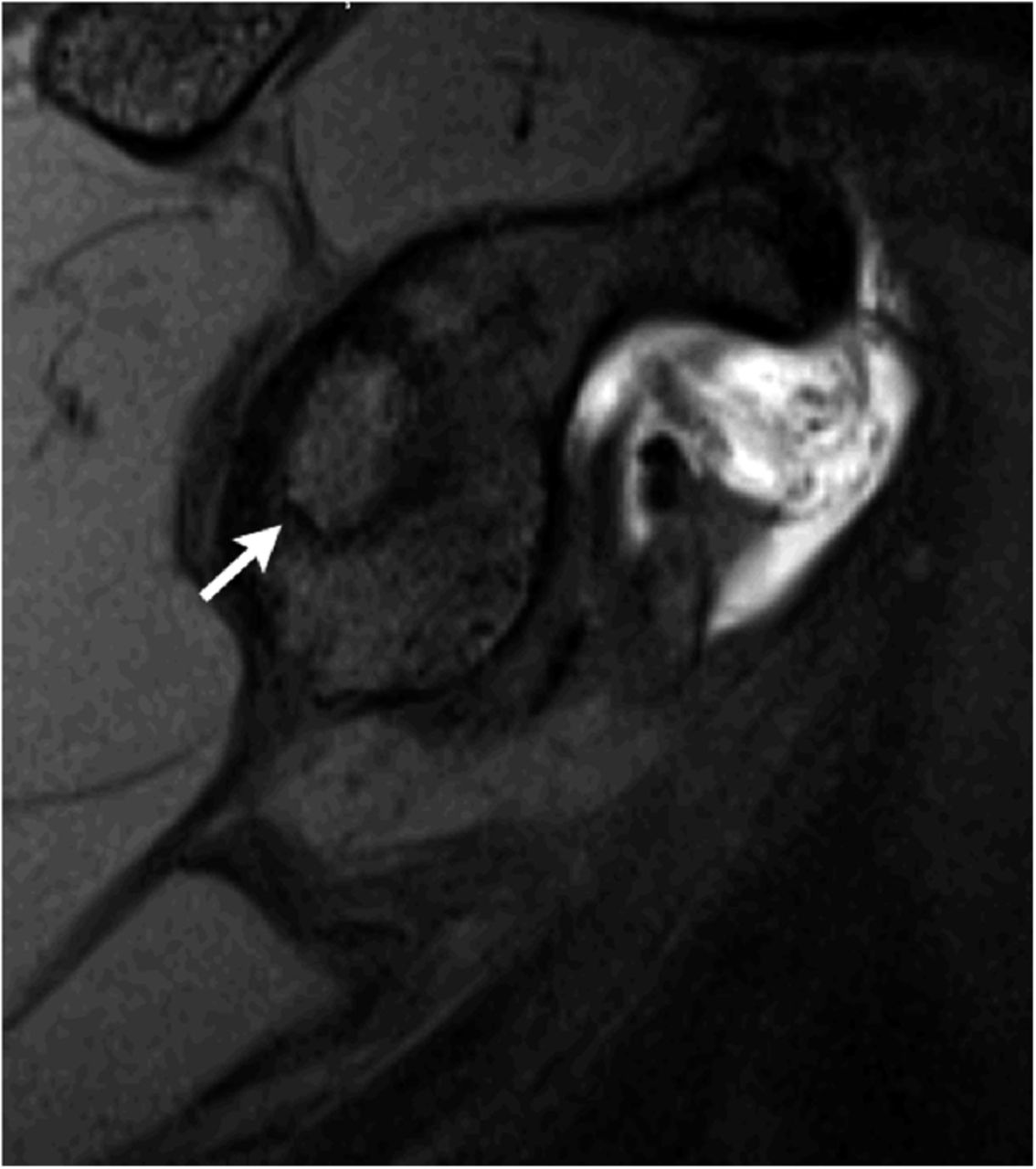
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3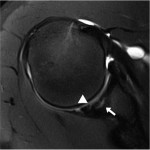 Fig. 4
Fig. 4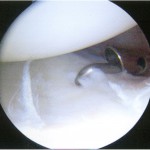 Fig. 5-A
Fig. 5-A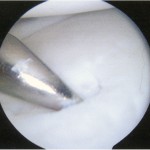 Fig. 5-B
Fig. 5-B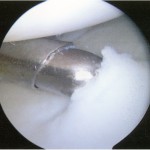 Fig. 5-C
Fig. 5-C Fig. 5-D
Fig. 5-D Fig. 5-E
Fig. 5-E