A Fifty-four-Year-Old Man with Chronic Lower Back Pain
September 16, 2015
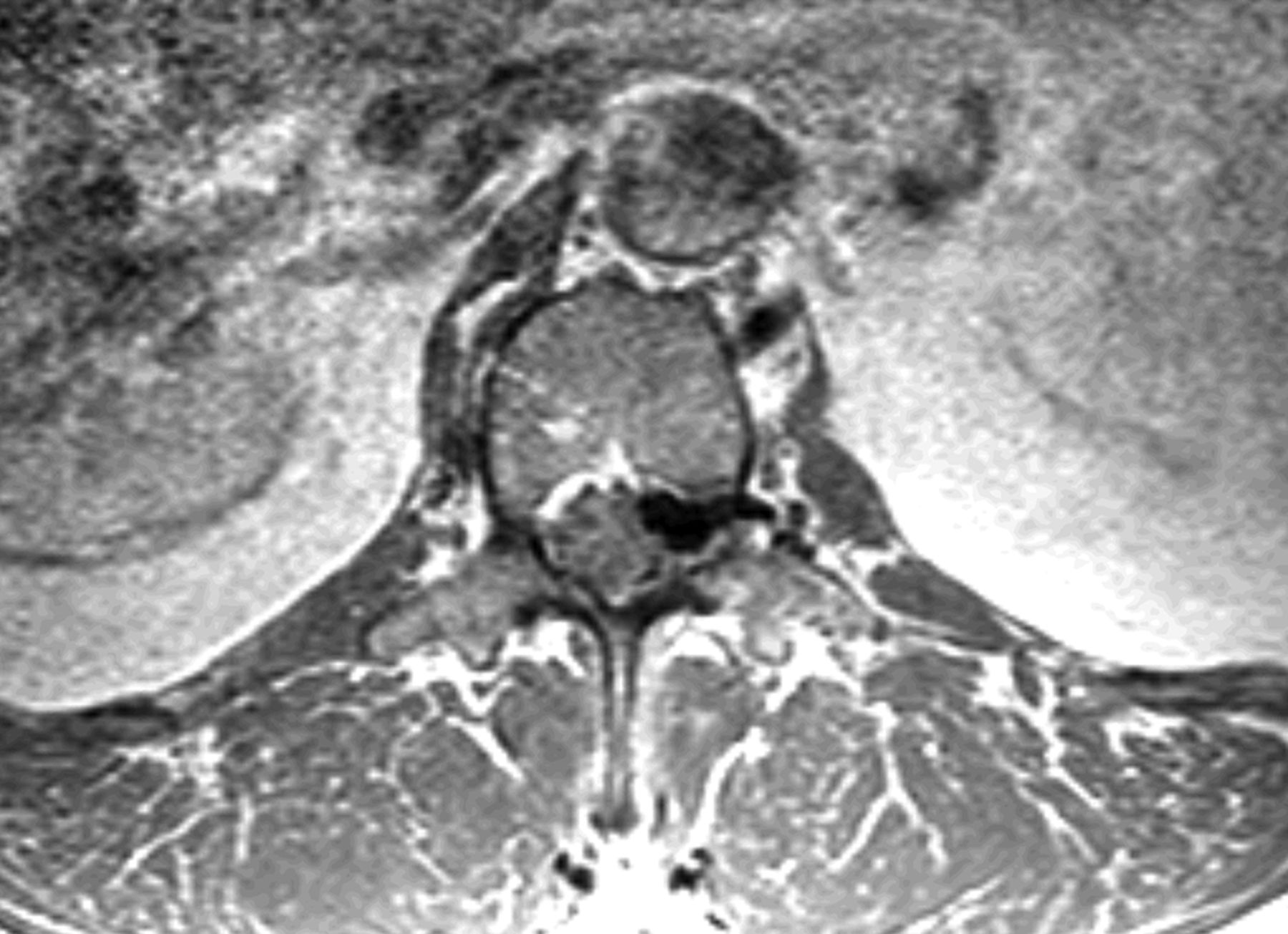
A fifty-four-year-old man presented to our office with chronic low back pain and new-onset left lower-extremity radiculopathy radiating from the buttock to the anterior proximal part of the thigh (L2 distribution). His symptoms were exacerbated with activity and sitting but were alleviated with rest and by lying supine. There were no motor deficits or symptoms involving the bowels or bladder on presentation. The patient’s medical history was remarkable for mild scoliosis, kidney disease, and a thyroid disorder. His surgical history was negative for any spinal surgery or trauma, and the patient indicated that he did not use alcohol or tobacco. On physical examination, the patient appeared well, was afebrile, and had stable vital signs. Musculoskeletal examination revealed spinal extension that was limited to 75% of normal. Neurological examination revealed full strength in both lower extremities, with the exception of grade-4 (of 5) strength with flexion of the left hip. Reflexes and sensation to light touch were intact. The patient exhibited no gait abnormalities. Magnetic resonance imaging (MRI) performed one month prior to the examination revealed what initially appeared to be a large disc extrusion at the L1-L2 level causing severe neural foraminal narrowing and compression of the left L2 nerve root as well as a moderate disc herniation at the L2-L3 level. However, after further review with the spine and radiology teams, it was determined that the neural foraminal compression could be caused by a disc extrusion with coexisting facet joint hypertrophy. The MRI also revealed moderate to severe spinal stenosis at the L4-L5 level, with multilevel degenerative disc disease (Figs. 1-A and 1-B). Repeat MRI demonstrated disc desiccation with symmetrical disc bulging at the L1-L2 disc space. Additionally, there was an epidural rim enhancement on T2 imaging, which was presumed to be an extruded free disc fragment (Fig. 2). The patient elected to undergo a left-sided L1-L2 neuroforaminal decompression and partial discectomy. A 3-mm Kerrison rongeur was used to perform a laminectomy at L1 and L2. Lateral recess decompression was performed bilaterally at L1-L2 using a 2-mm Kerrison rongeur, removing the ligamentum flavum and performing a partial medial facetectomy. While performing a midline L1-L2 discectomy, a disc extrusion was noted but this was not a large herniation. Brisk and persistent bleeding was encountered on decompressing the lateral recess and neuroforamen; this required extensive electrocautery in addition to Gelfoam sponge (Upjohn) and FloSeal (Baxter) to achieve hemostasis. The discectomy ultimately resulted in total blood loss of 2 L. Tissue for biopsy was sent for pathologic examination; however, the material was collected from the midline disc extrusion and ligamentum flavum prior to decompressing the lateral recess and encountering the substantial bleeding. The biopsy specimen was determined to be benign fibrous tissue, consistent with a vertebral disc. The patient’s initial postoperative course was uneventful. However, ten weeks after the discectomy, he returned for follow-up evaluation reporting recurrent low back pain (7 on a scale of 0 to 10) with left-sided radiculopathy. MRI results were noted.
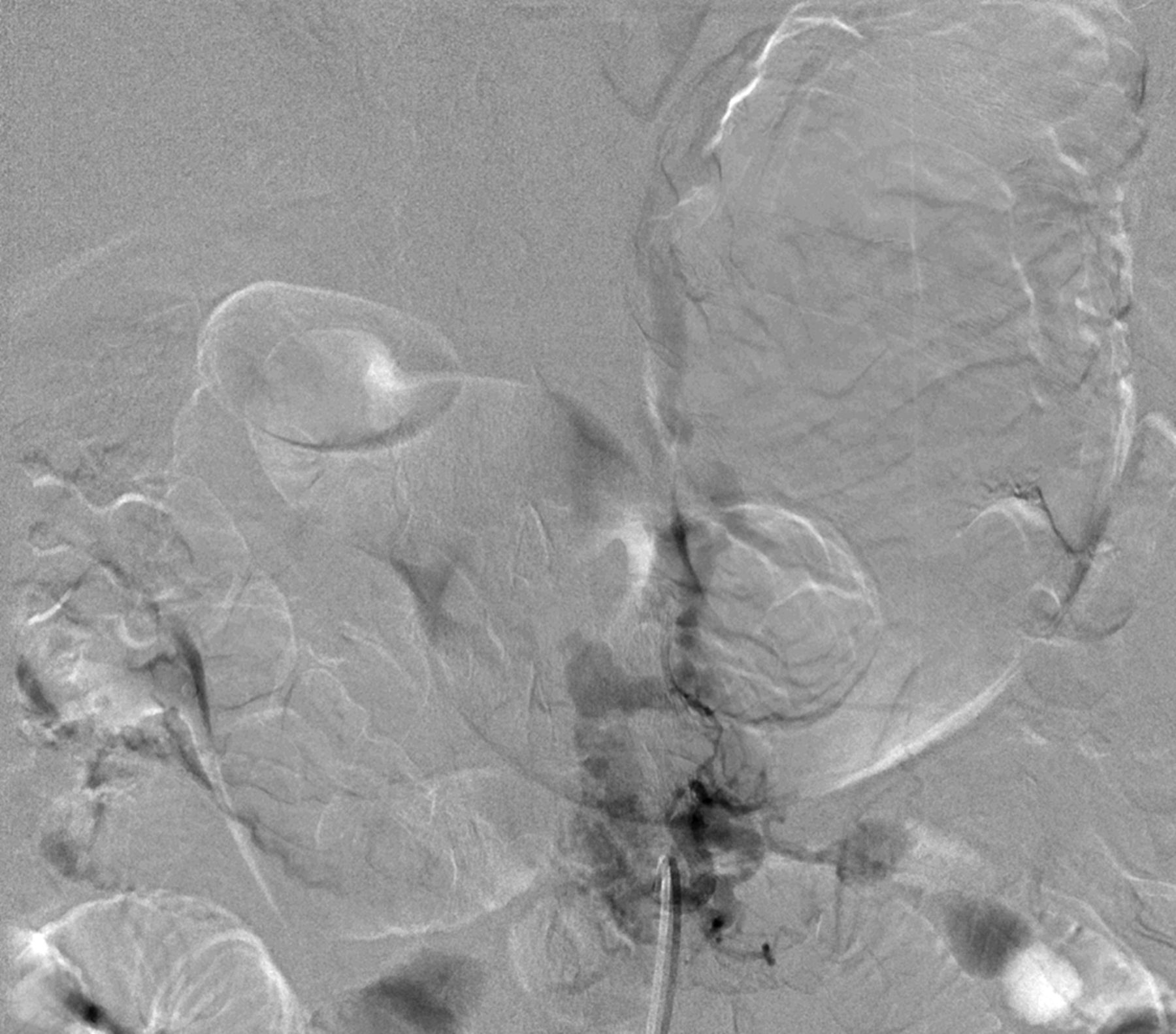
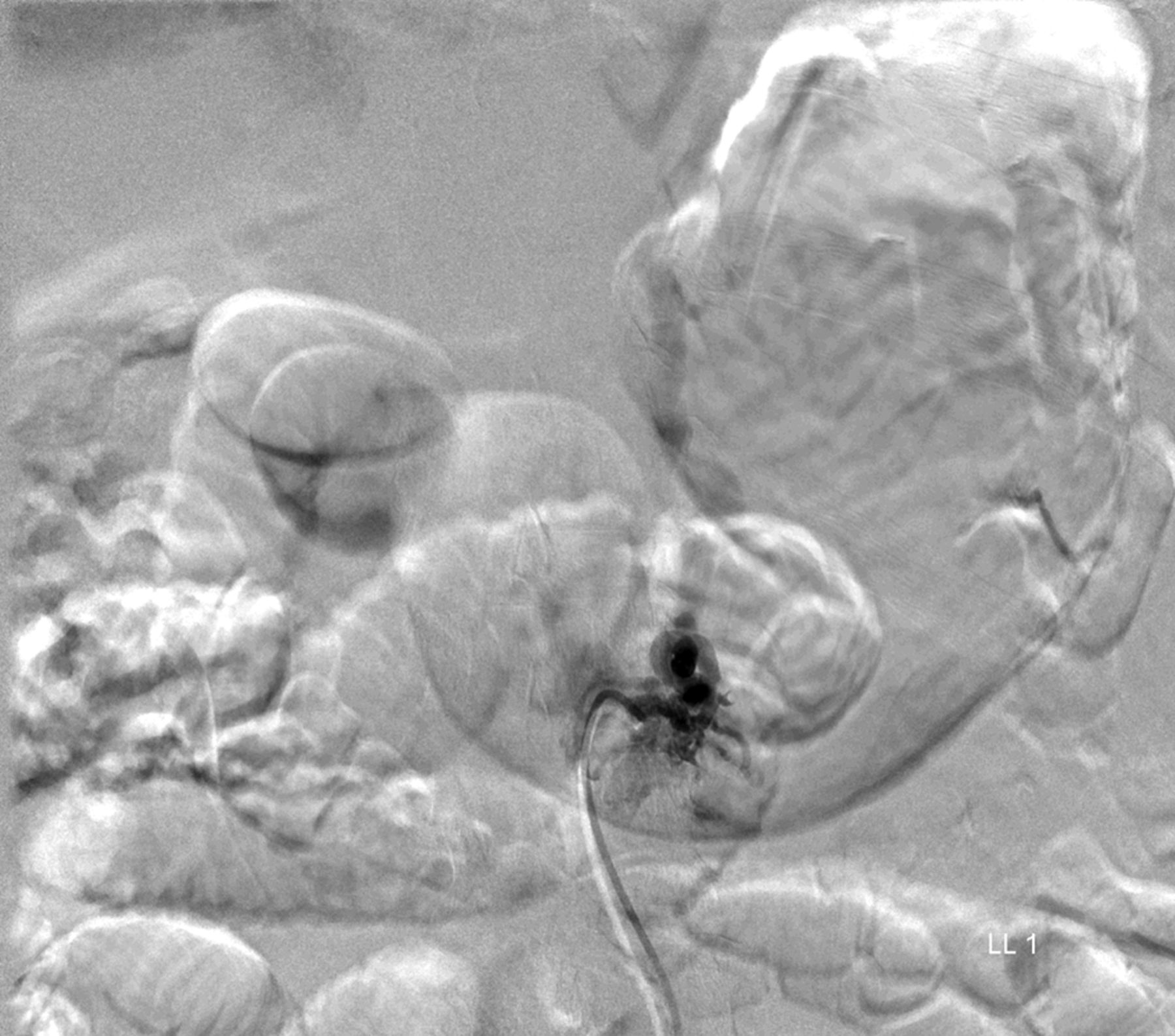
MRI with contrast at this time again demonstrated a lobular focus of low signal on T1 and T2-weighted images at L1-L2 extending into the neuroforamen, similar to prior imaging studies (Fig. 3). The radiology report suggested a new disc extrusion accompanied by a complex synovial cyst (versus pigmented villonodular synovitis). However, because of the persistent bleeding encountered during the initial discectomy, there was concern for a vascular etiology. Therefore, the neurosurgical team performed a transfemoral spinal angiogram with selective right L1 and L2 segmental artery catheterization. Multiple imaging runs showed a spinal dural arteriovenous fistula (SDAVF) with early venous drainage and multiple small racemic feeders. Additionally, the right L2 segmental artery demonstrated multiple feeders through the SDAVF (Figs. 4-A and 4-B). A revision decompression was performed with bilateral L1 and L2 laminectomy as well as microsurgical resection of the SDAVF with durotomy and cauterization. The postoperative course was uneventful. At one year after presentation, the patient had made a full recovery. He had returned to work full time as a manual laborer, with no recurrence of the axial back pain or lumbar radiculopathy. Neurological examination revealed grade-5 strength in all distributions in both lower extremities, with no residual sensory deficits.
Proceed to Discussion >>Reference: Verma K, Fennessy J, Huang R, Jabbour P, Rihn J. Spinal dural arteriovenous fistula presenting as a recurrent nucleus pulposus herniation: a case report and literature review. JBJS Case Connect. 2015 Jul 08;5(3):e59.
The exact etiology of SDAVF is still not fully understood, although it is widely accepted to be an acquired disease with risk factors that are multifactorial. Of the myriad possible triggering events, infection, syringomyelia, trauma, and surgery have been the most commonly observed. In 1992, Anson and Spetzler proposed a classification system that divided spinal vascular malformations into four types, with type 1 indicating a dural arteriovenous fistula; type 2, an intramedullary glomus-type arteriovenous malformation; type 3, an intramedullary juvenile-type arteriovenous malformation; and type 4, an intradural, extramedullary arteriovenous fistula. Type-1 SDAVFs are subcategorized into type 1A (single feeding artery) and type 1B (multiple feeding arteries). Most SDAVFs are intradural or within the nerve root sleeve. The venous engorgement within the nerve root sleeve traversing the neuroforamen explains the neuropathic symptoms commonly associated with the initial presentation. The most common presenting symptoms reported in association with SDAVF are limb weakness (42.9%), decreased sensation in the lower extremities (20.1%), pain (9.7%), paresthesias (8.5%), and sphincter dysfunction (4.6%). A mean age of sixty-three years at presentation has been reported, with 78% of patients being male. With this constellation of symptoms mimicking common lumbar spine pathology, there is often a one to two-year delay in appropriate diagnosis, as well as considerable risk for inappropriate and invasive intervention, which occurs in 10 to 22% of cases. Wang et al. demonstrated misdiagnosis in >81% of SDAVF cases on initial evaluation, leading to inappropriate and invasive intervention in more than half of those patients. Review of the literature suggests that T2-weighted MRI of the spine of patients presenting with undiagnosed SDAVF will demonstrate cord signal changes in 73% to 93% of cases. According to the classification described above, our patient had a type-1B SDAVF. MRI demonstrated what appeared to be a disc herniation into the neural foramen at the L1-L2 disc space. This led the region of signal intensity in the disc space on T2-weighted MRI to be mistaken for minor hemorrhage associated with a disc injury. In retrospect, the lateral recess stenosis was caused by an SDAVF with coexisting facet hypertrophy. With his nonspecific symptoms mimicking more common spine abnormalities, this patient’s diagnosis was a challenge for spine surgeons with both orthopaedic and neurosurgical training. In patients with MRI signal suggestive of vascular malformations (T2 hyperintensity in the lower spinal cord and conus medullaris), MR angiography has a 95% positive predictive value for diagnosing SDAVF. Early diagnosis may improve clinical outcomes for these patients and potentially avoid open surgical decompression and the risk of severe hemodynamic complications. Although no substantial vascular abnormality was noted during surgery in the present case, we believe that any patient with profuse, unexplained bleeding intraoperatively should be resuscitated, stabilized, and evaluated with MR angiography. Since many of these patients are being managed in a surgical center or outpatient setting, rapid identification and procurement of blood products may be life-saving. Once appropriately diagnosed, surgical ligation leads to full resolution in up to 97% of patients, with improved or stable motor function. Following the microsurgical cauterization of the L1 and L2 fistulae, our patient improved clinically, with decreased foraminal stenosis on radiographic imaging at the two-week follow-up. In addition, at six months and one year of follow-up, the patient remained free of axial back pain or radiculopathy. He returned to work full time as a manual laborer. Patients with persistent symptoms after surgical ligation may warrant additional MR angiography. For these patients, open surgical decompression should be approached with caution.
Reference: Verma K, Fennessy J, Huang R, Jabbour P, Rihn J. Spinal dural arteriovenous fistula presenting as a recurrent nucleus pulposus herniation: a case report and literature review. JBJS Case Connect. 2015 Jul 08;5(3):e59.
Recurrent disc herniation
Synovial cyst
Spinal dural arteriovenous fistula
Spinal cord tumor
Neurofibromatosis


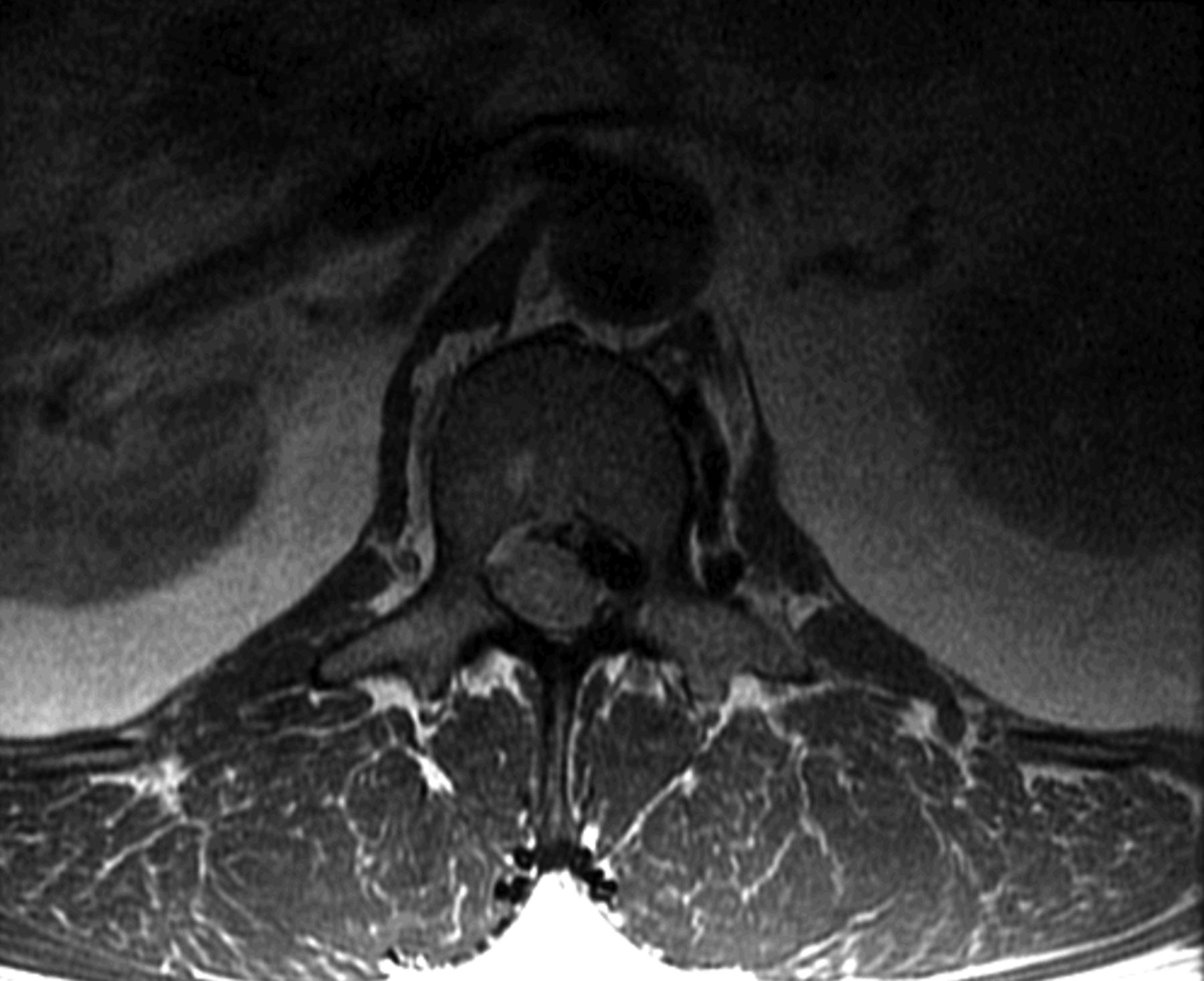
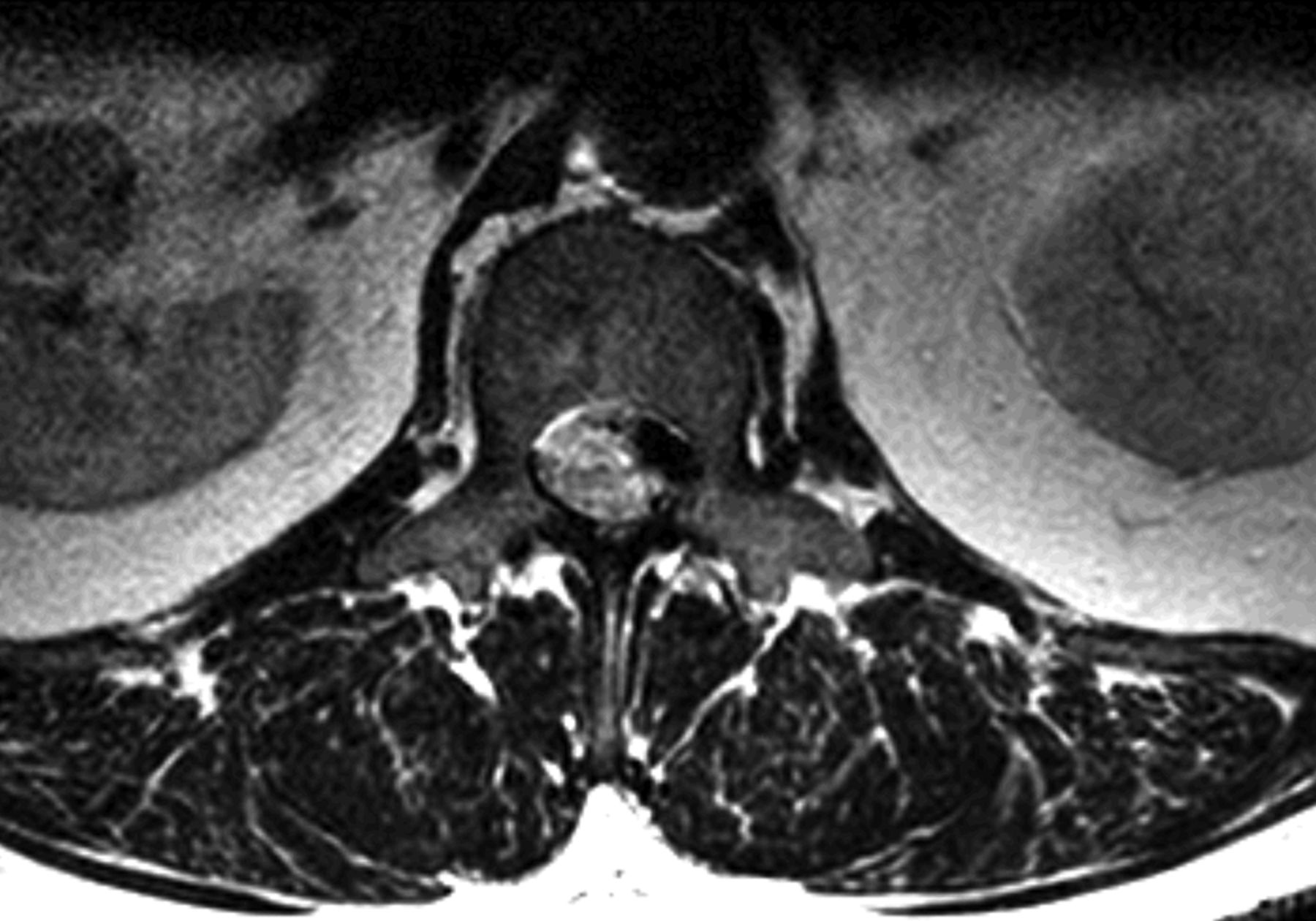
 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2
Fig. 2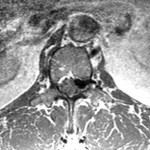 Fig. 3
Fig. 3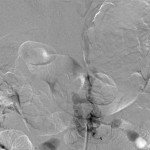 Fig. 4-A
Fig. 4-A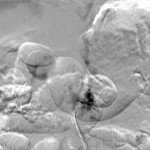 Fig. 4-B
Fig. 4-B