A Forty-two-Year-Old Man with Shoulder Weakness Following a Seizure
November 4, 2015
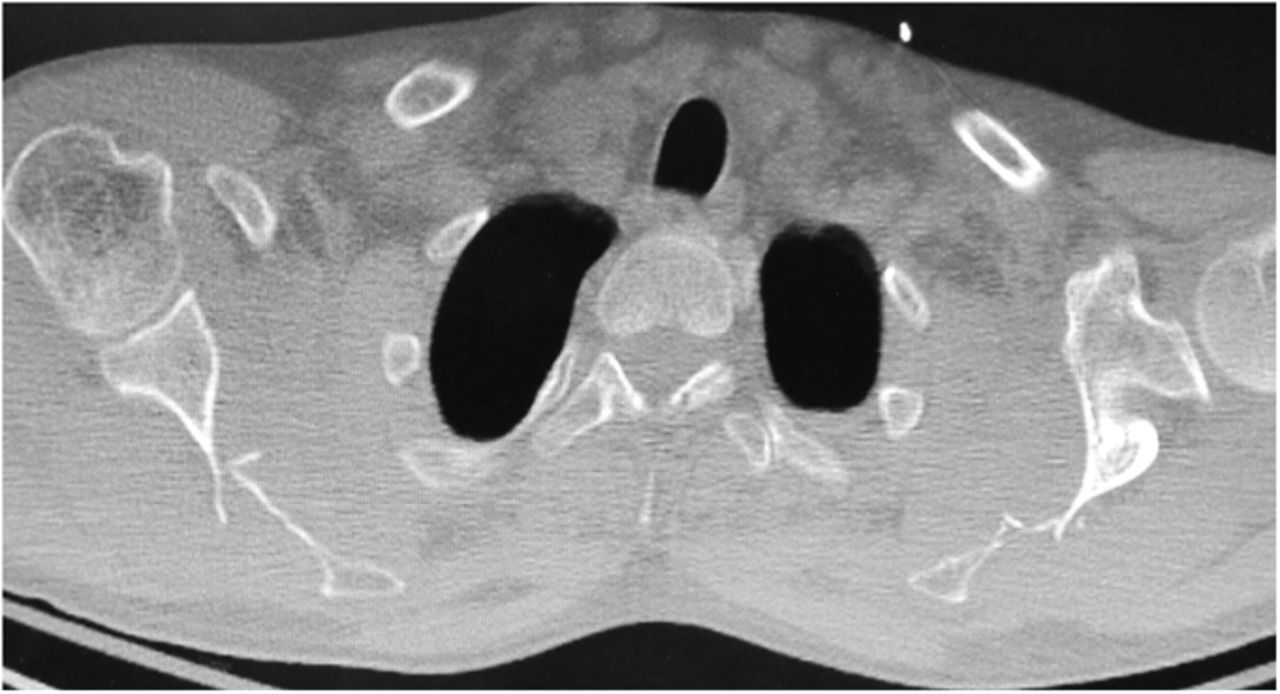
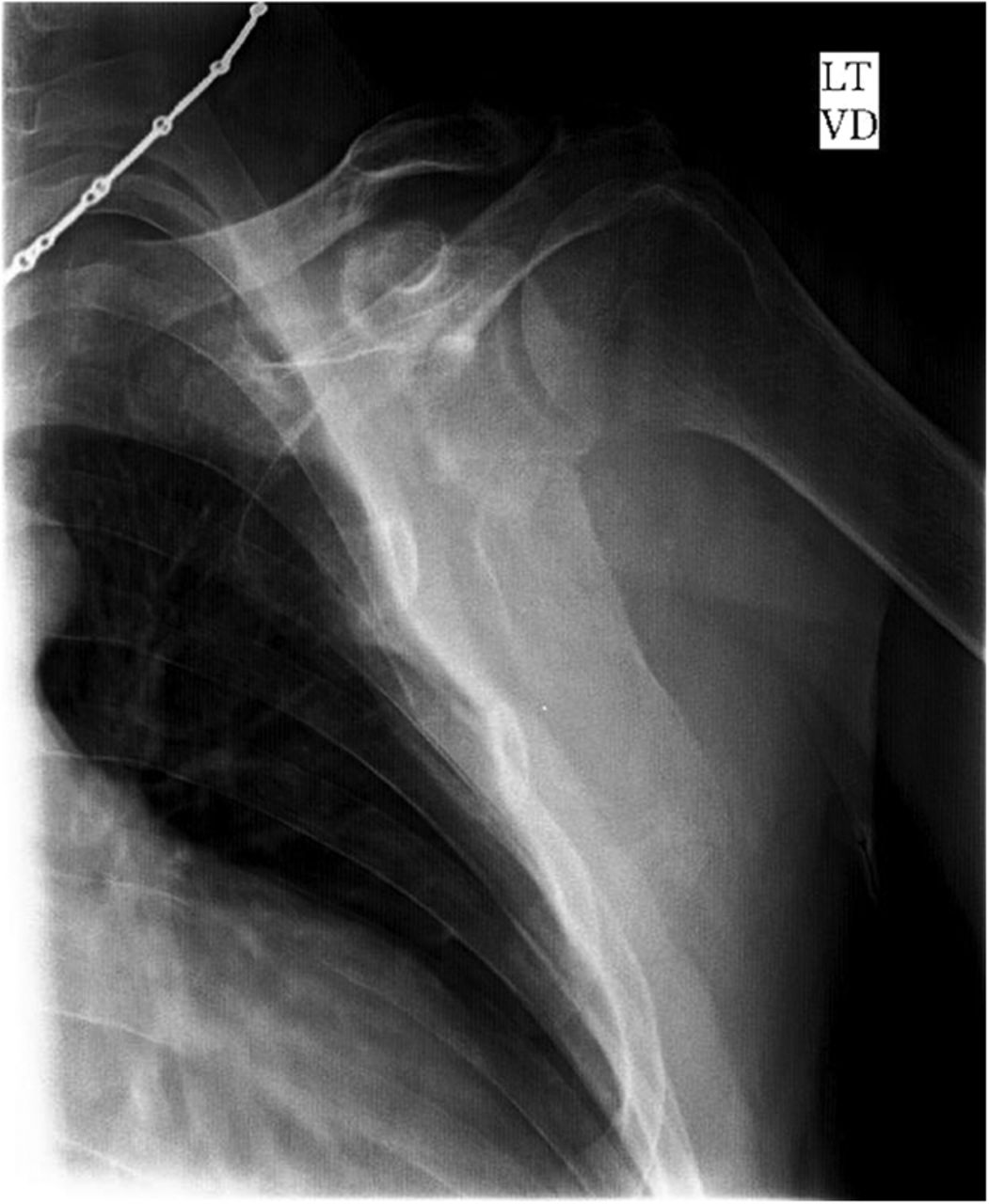
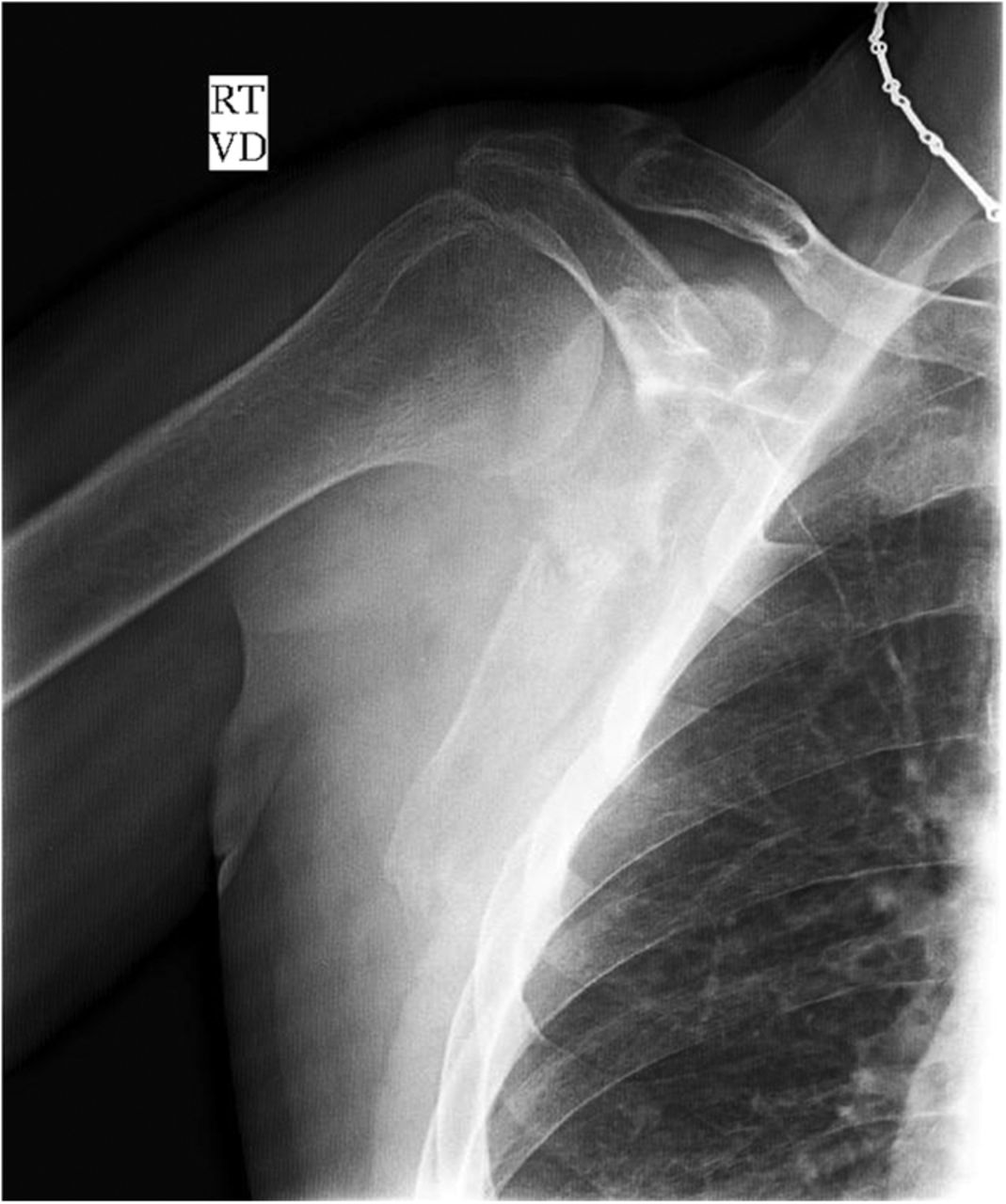
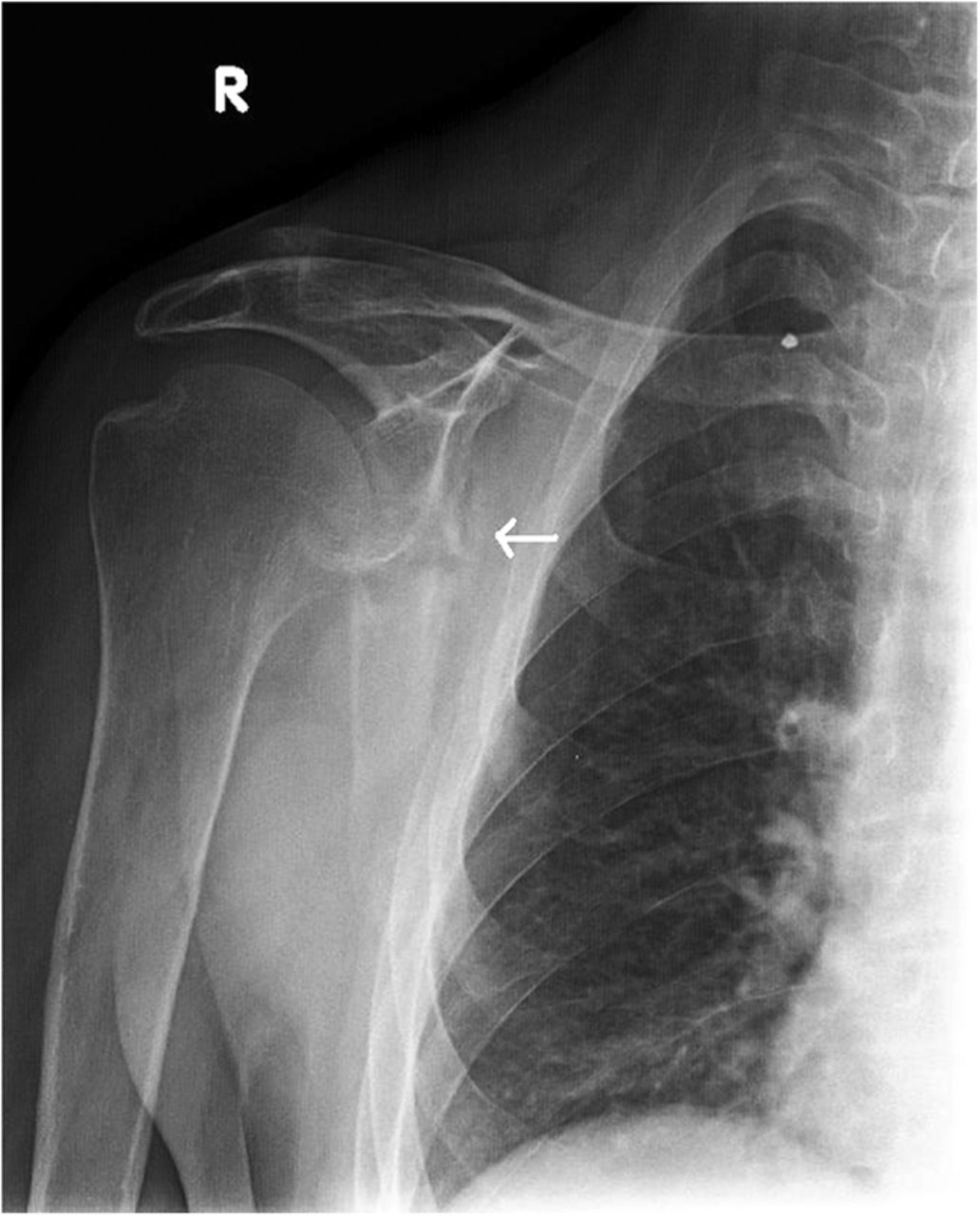
A forty-two-year-old left-hand-dominant man was admitted to the intensive care unit with profound hyponatremia after a witnessed, single, generalized tonic-clonic seizure following a missed dialysis appointment. The chief symptom was bilateral upper-extremity weakness and limited shoulder motion, which occurred immediately after the seizure. Medical history was notable for hypertension, gout, and polycystic kidney disease with chronic renal failure that required hemodialysis. Medication included 2000 mg of calcium acetate three times per day for hyperphosphatemia. One week prior to the seizure, the patient had hypocalcemia (calcium, 6.0 mg/dL) and hyperphosphatemia (phosphate, 8.9 mg/dL), and two weeks prior to the seizure, the parathyroid hormone level was 1900 pg/mL. In the laboratory values on admission, hyponatremia, hypocalcemia, and hyperphosphatemia were all present. Radiographs and computed tomography (CT) of both shoulders (Figs. 1 and 2), with axial and coronal reconstructions, were made.
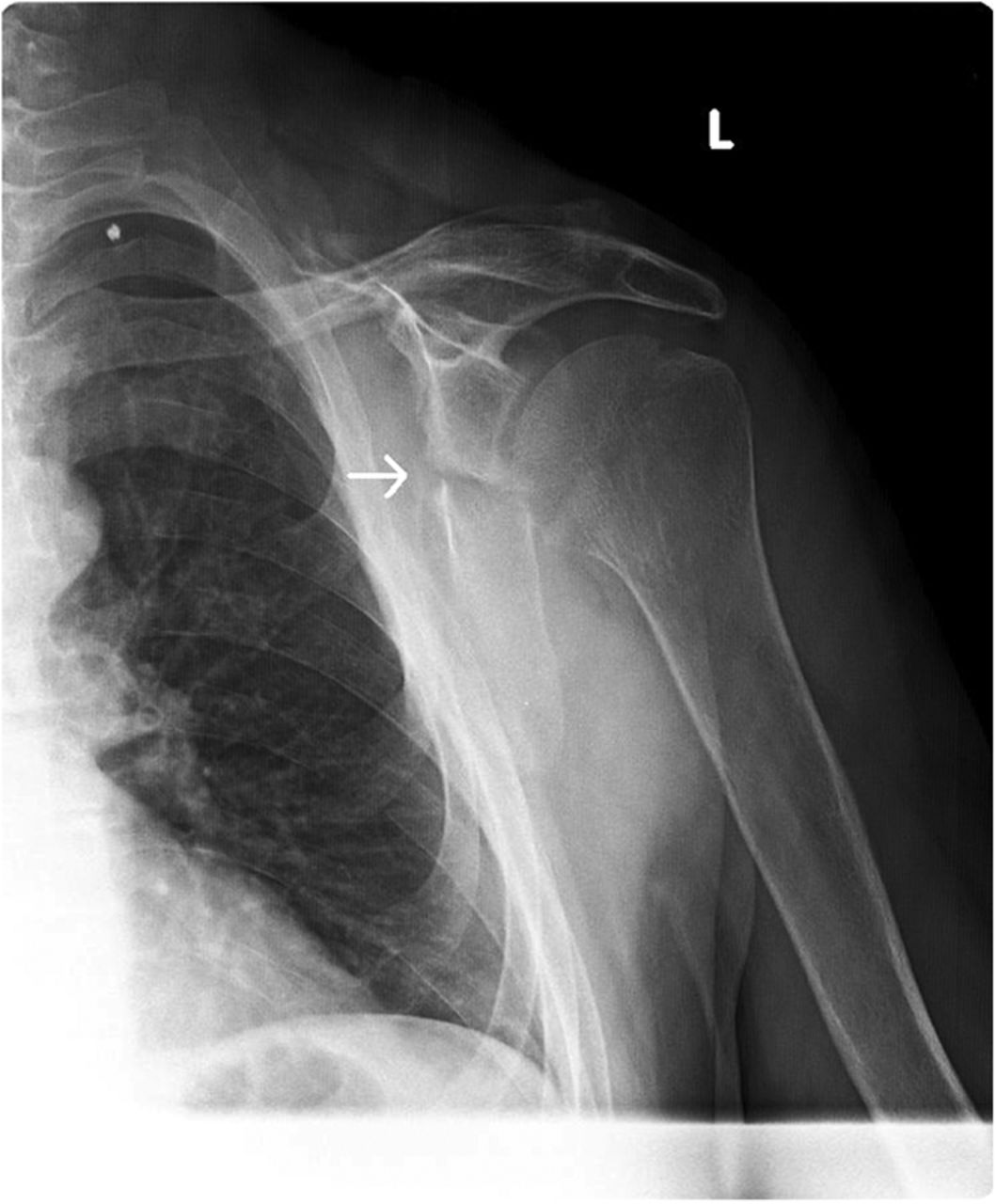
The imaging studies demonstrated comminuted fractures of the scapulae inferior to the glenoid (Orthopaedic Trauma Association [OTA] classification 14-A3.2). Left scapular images showed fractures of the spine and body, with retroversion of the scapular spine in relation to the body. Images also showed comminution of the scapular body without substantial displacement or overlap (Figs. 1, 2, and 3). On the right scapula, the superior fracture site was angulated with the fracture angle apex oriented posteriorly, with slight overlap of the scapular spine posterior to the body. Images also showed comminution of the scapular body angulated with the fracture angle apex oriented posteriorly, without substantial displacement or overlap (Figs. 1 and 4). Radiographs of the left elbow demonstrated swelling and calcification within the soft tissues posterior to the humeral condyles. The left shoulder was immobilized, the right arm was placed in a sling, and the patient was instructed to follow up as an outpatient. The patient presented to the office at four weeks following the initial seizure episode with symptoms of persistent right scapular pain and limited motion of both shoulders. Bilateral scapular radiographs revealed persistent fracture lines with evidence of healing of both scapular fractures (Figs. 5 and 6). Symptoms also included persistent weakness at both elbows; the left was more severe than the right. Physical examination confirmed extensor weakness and palpable soft-tissue defects consistent with a complete left triceps tendon tear and a partial right triceps tendon tear. Bilateral elbow radiographs demonstrated calcification proximal to the insertion of the triceps bilaterally (Figs. 7 and 8). Magnetic resonance imaging (MRI) of the dominant left elbow evaluated for triceps tendon rupture to determine the appropriate management. MRI of the right elbow was not obtained because the physical examination was consistent with the diagnosis of partial triceps tear, and surgical management of both elbows would have necessitated simultaneous complete immobilization and increased impairment in the activities of daily living. Therefore, the best course of management for the nondominant arm was nonsurgical limitation in movement with physical therapy. MRI of the left elbow demonstrated a complete rupture of the distal part of the triceps with retraction, soft-tissue swelling, and fluid accumulation at the site of triceps insertion. An open repair of the distal part of the left triceps tendon was performed. A posterior incision and exposure revealed a thin ruptured triceps tendon with proximal migration, myxoid degeneration, and tophus material by visual analysis. The triceps was repaired with use of an end-to-end anastomosis without tension, with a modified Kessler technique with use of one suture anchor into the olecranon and nonabsorbable suture. Postoperative injection of Marcaine (bupivacaine hydrochloride) with epinephrine was provided, and the elbow was immobilized in a splint in extension with instructions to follow up in two weeks. At the two-week postsurgical follow-up, the patient had active extension of the left elbow with slight discomfort. At that time, the patient’s scapular pain was markedly diminished, and bilateral shoulder radiographs showed callus formation at each fracture site (Figs. 9 and 10). The patient was lost to additional follow-up.
Proceed to Discussion >>Reference: Henry JE, Beveridge RE, Horner I. Bilateral scapular fracture and triceps tendon rupture after a grand mal seizure: A case report. JBJS Case Connect, 2013 Apr 10;3(2):e35.
Renal osteodystrophy is a common complication of chronic renal failure, clinically manifested as pruritus, bone pain, weakness, muscle wasting, and metastatic calcification. The mechanism of renal osteodystrophy is complex, and leads to osteitis fibrosa, osteomalacia, and osteosclerosis. The major forms of bone pathology in chronic renal failure patients are osteitis fibrosa secondary to hyperparathyroidism and vitamin D-resistant osteomalacia. Secondary hyperparathyroidism causes alterations in calcium and magnesium metabolism that can increase susceptibility to fracture as well as induce seizure activity and muscle spasticity, thus leading to pathologic fractures. Mathews et al. reported that forceful muscle contractions during a grand mal seizure can injure the scapula in osteodystrophic patients. Scapular fractures are commonly caused by high-energy trauma, electric shock, or convulsions. There are several published cases of bilateral and unilateral scapular fracture secondary to seizure activity, as well as bilateral scapular fracture secondary to electric shock. Forceful muscle contractions during a seizure can injure the scapula and increase the susceptibility to triceps tendon rupture in osteodystrophic patients. Tendon rupture in chronic renal failure patients often occurs in weight-bearing tendons; the triceps brachii is the most common tendon of the upper extremity that is injured. Tendon rupture of the distal part of the triceps or tendon avulsion is an uncommon injury, most often associated with anabolic steroid use, weight lifting, or direct laceration. A search of the current literature identified only one case report of bilateral partial triceps tendon rupture in an athlete, three cases of bilateral complete triceps tendon rupture in hemodialysis patients, and only two reported cases of unilateral triceps tendon rupture secondary to seizure activity. Many authors have postulated that there is an association of tendon rupture with primary hyperparathyroidism, indicating an increased risk with the subsequent use of quinolone antibiotics or anabolic steroids. An increased risk of tendon rupture in chronic renal failure patients with secondary hyperparathyroidism is believed to be secondary to the weakness of the bone-tendon junction due to increased osteoclastic cortical bone resorption. Searfoss et al. hypothesized that prolonged hyperparathyroidism may result in tendinous ground-substance membrane changes that predispose tendons to rupture. In a case report, Mont et al. suggested that hypocalcemic tetany induced a spontaneous triceps tendon avulsion and bilateral quadriceps tendon rupture in a patient. Murphy and McPhee suggested that spontaneous tendon rupture occurs secondary to degeneration of the tendon due to chronic acidosis, leading to elastin deposition in the tendons that predisposes them to rupture. Beta-2 microglobulin amyloidosis has also been listed as a potential source of tendon rupture in patients with renal failure. In our patient, serum parathyroid hormone level was markedly increased two weeks prior to the injury, which supports a theory suggesting complications of hyperparathyroidism as a proposed etiology of spontaneous tendon rupture in a patient with chronic renal failure. Triceps ruptures are often misdiagnosed as inflammatory processes. Delay to diagnose the triceps tendon ruptures in our patient was attributed to the severe bilateral scapular pain secondary to the fractures. This case reinforces the importance of considering the possibility of tendon rupture resulting from a seizure or fall in patients with chronic renal failure and secondary hyperparathyroidism. In conclusion, patients in chronic renal failure with hypocalcemia and hyperparathyroidism are prone to develop fractures and tendon injuries. It is important to recognize the common musculoskeletal complications that can occur in these patients in an attempt to prevent and correctly diagnose these injuries. This unique case report further stresses the importance of thorough clinical evaluation with physical examination and imaging for tendon rupture and pathologic fracture when a patient with chronic renal failure presents with symptoms of inflammation, pain, decreased range of motion, or any combination thereof following a seizure.
Reference: Henry JE, Beveridge RE, Horner I. Bilateral scapular fracture and triceps tendon rupture after a grand mal seizure: A case report. JBJS Case Connect, 2013 Apr 10;3(2):e35.
Bilateral scapular body fractures
Brown tumors of the scapulae
Scapulothoracic dissociation bilateral
Aneurysmal bone cysts of the scapular body
Bilateral scapular body simple bone cysts

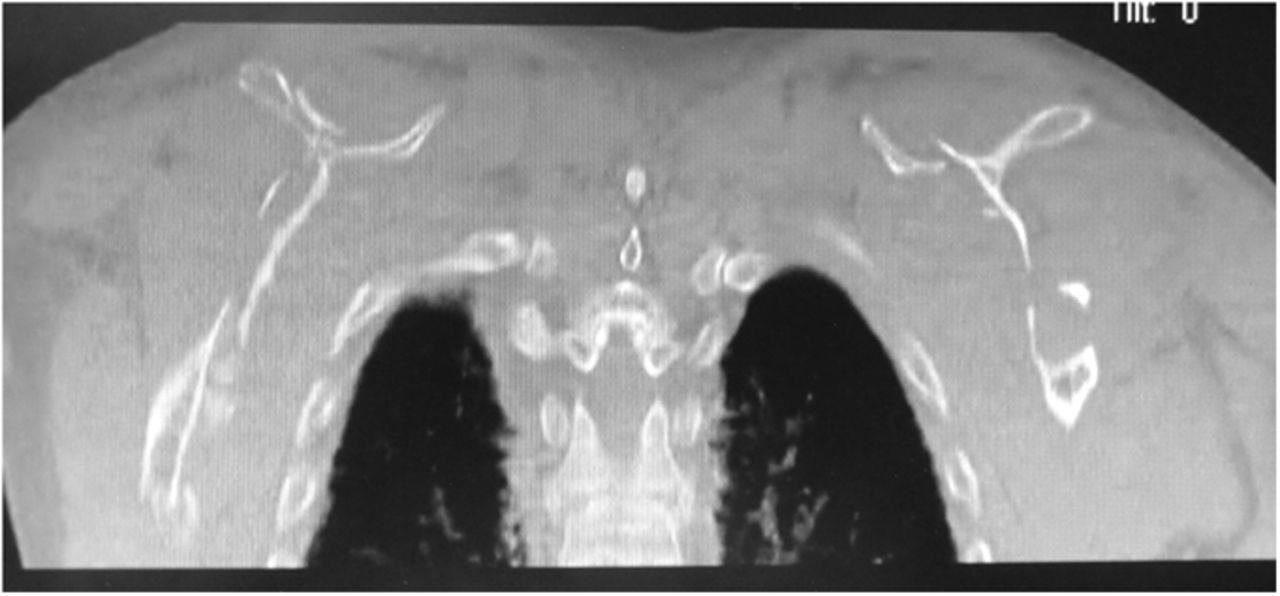
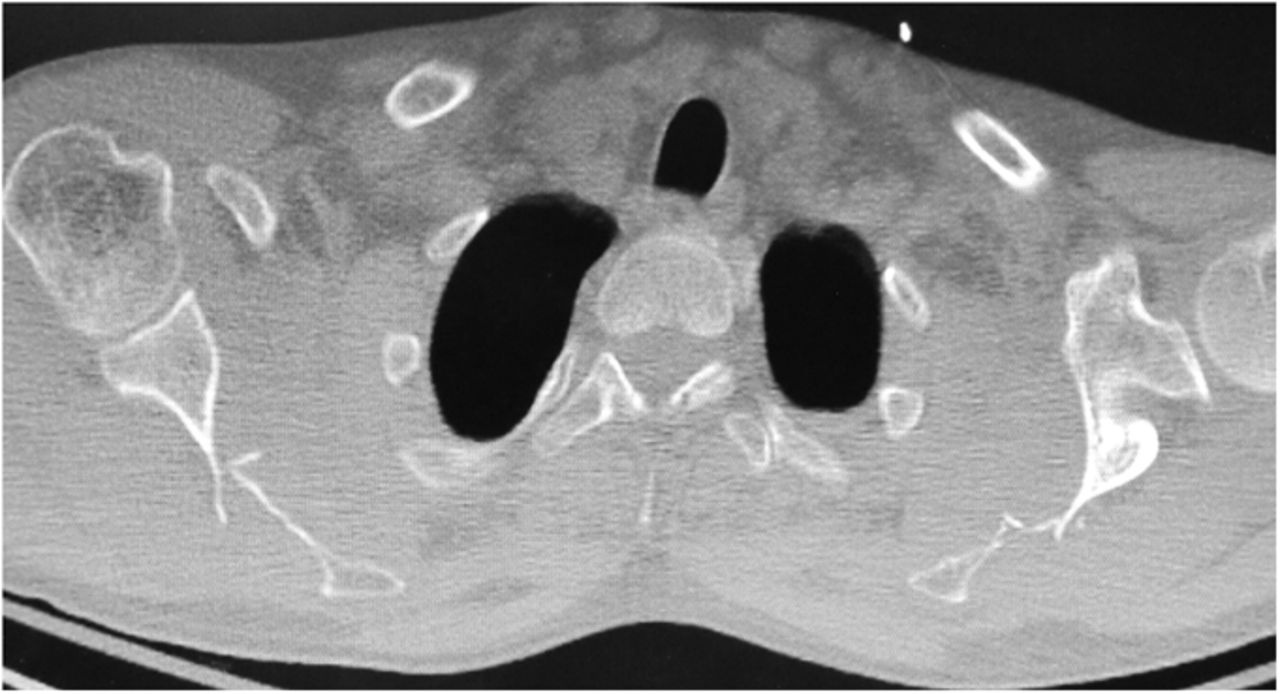
 Fig. 1
Fig. 1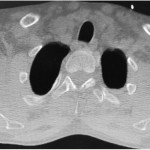 Fig. 2
Fig. 2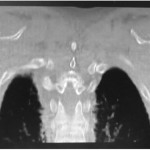 Fig. 1
Fig. 1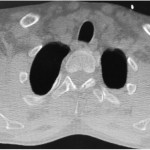 Fig. 2
Fig. 2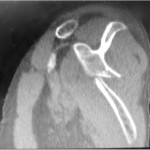 Fig. 3
Fig. 3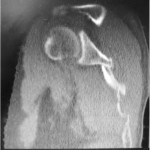 Fig. 4
Fig. 4 Fig. 5
Fig. 5 Fig. 6
Fig. 6 Fig. 7
Fig. 7 Fig. 8
Fig. 8 Fig. 9
Fig. 9 Fig. 10
Fig. 10